Case Study – A Tiny Heart
( \newcommand{\kernel}{\mathrm{null}\,}\)
Kelly was in the maternity ward, her contractions were about 3 minutes apart and the fetal monitor was sounding frequent beeps giving indications of the baby’s heartbeat. The external monitor was attached via a large belt strapped around Kelly’s abdomen. It also recorded the intensity and frequency of the contractions.
Doctor Tavish entered the room carrying a clipboard. He checked the monitor and nodded, giving Kelly assurances that everything looked alright. “It won’t be long now,” he said. “Little Lucas is probably very anxious to meet his new family.” Kelly looked nervous though, her contractions had begun a few weeks before her due date. Though the doctor insisted that everything should be fine, she couldn’t help but worry.
Kelly’s husband, Chris, was sitting in a chair nearby and he looked nervous. “Why does the heart rate change every time Kelly has a contraction?”
The doctor reviewed the monitor. “The baby is under some stress, but it’s nothing to be concerned about, the heart rate is strong and he’s getting enough oxygen. If anything changes, we’ll re-evaluate.”
The doctor returned about 20 minutes later after Kelly’s labor hadn’t progressed any further. He explained that the nurses had alerted him to irregularities in the baby’s heartbeat that indicated that Lucas was under stress and perhaps not getting enough oxygen. “I think it’s time we consider Caesarean section.” He said. The parents decided to go with the doctor’s suggestion, and Kelly was quickly taken to the operating room.
Data: Fetal Monitor
|
Monitor Readings |
At Rest |
During Contraction |
After contraction |
|
1 |
120 bpm |
150 bpm |
115 bpm |
|
2 |
125 bpm |
160 bpm |
110 bpm |
|
3 |
125 bpm |
160 bpm |
115 bpm |
|
4 |
140 bpm |
170 bpm |
90 bpm |
|
5 |
150 bpm |
175 bpm |
90 bpm |
- Create a graph showing Lucas’ heart rate from monitor readings. Be sure to label the X and Y axis and the three lines.
- Do an internet search to find out what a normal fetal heart rate is? At what point in the graph would the doctor have become concerned (circle)?
Part II: The Delivery
An hour later, baby Lucas was delivered. Kelly had been given an epidural and was awake during the delivery. When Lucas first arrived, the doctors whisked him away to make sure he was clean and stabilized. When the nurse brought Lucas back, Kelly was able to see him for a brief time, Doctor Tavish was still worried.
“We are going to take Lucas for more tests. His breathing is fast and he appears to be cyanotic.” Kellie looked surprised, “Cyanotic! That sounds terrible!.” The doctor held up a Lucas’ tiny hand, “see how his fingers are blue, that’s what it means to be cyanotic. Lucas isn’t getting enough oxygen.
Chris and Kelly were very worried, though Doctor Tavish reassured them that it is not unusual for newborns to have breathing difficulties. “We just want to make sure his heart is functioning correctly.” “His heart?” Asked Chris. “I thought you said he was having trouble breathing, why would you need to check his heart?”
Doctor Tavish pulled out a diagram of the heart and the lungs to show Chris how the two organs work together to oxygenate the blood. “We need to find out if Little Lucas has a problem with his heart or a problem with his lungs.”
- Define epidural:
Define cyanotic:
Why would a cyanotic baby have a fast breathing rate?
- Draw a diagram of the heart of a human adult like the one Dr. Tavish showed Chris. Sketch a heart and label the main vessels and chambers. Use arrows to show the flow of blood.
- Before birth, the fetal circulatory system includes three open structures through which blood moves that normally close soon after birth. These structures are the ductus arteriosus, the ductus venosus, and the foramen ovale. The foramen ovale allows the shunting of blood from the right atrium into the left atrium.
Before birth, much of a fetus's blood goes through a passageway (ductus arteriosus) between the aorta and pulmonary artery because the lungs are not yet in use. This passageway should close soon after birth, so the blood can take the normal route from heart to lungs and back. If it doesn't close, blood doesn't flow correctly. Use google IMAGE search on “fetal circulation.” *Edit your heart drawing to show the location of the foramen ovale.
- Why is the pulmonary circulation reduced in the unborn human fetus? What is the foramen ovale?
Part III—The I.C.U
As Kelly was recovering from her C-section, Doctor Tavish returned with some bad news. Lucas had been taken to the Intensive Care Unit because he was not getting enough oxygen.
“Many newborns recover from an oxygen deficit once their lungs have become fully inflated and the fluid has been cleared. Lucas continues to breathe rapidly and his blood oxygen levels are low. We think there’s a problem with his heart.”
The table summarizes his vital signs.
|
Parameter |
Lucas |
Normal |
|
Color of fingertips and lips |
Blue (cyanotic) |
Pink |
|
Heart rate (b/m) |
160 |
120 |
|
Heart sounds |
Lub “click” dup |
Normal |
|
Blood Pressure |
85/55 |
110/70 |
|
*Arterial PO2 |
100 |
100 |
|
Behavior |
Lethargic; sleepy |
Normal |
|
Breathing |
Heavy, rapid, congested |
Normal |
|
Feeding |
Disinterested |
Normal |
*PO2 (partial pressure of oxygen) reflects the amount of oxygen gas dissolved in the blood. It primarily measures the effectiveness of the lungs in pulling oxygen into the bloodstream from the atmosphere.
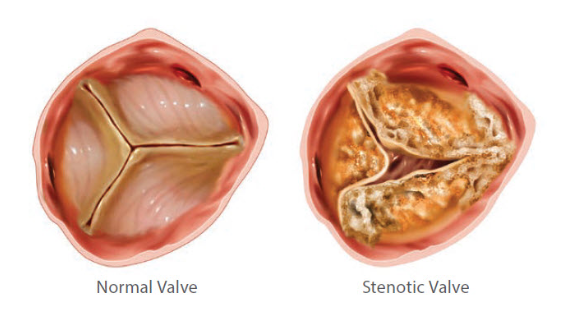
A cardiologist is brought in to determine what is wrong with Lucas’ heart. Doctor Brady performs an electrocardiogram to test for arterial stenosis, which he suspects due to the clicking sound of the heart. The sound is often caused by a thickened valve snapping into position. The electrocardiogram shows an enlargement of the left ventricle and restricted blood flow in the aorta. The ecg shows no evidence of a ventricular septal defect, a common heart defect seen in newborns.
Aortic stenosis is a term used to describe congenital heart defects that obstruct blood flow from the heart to the body. Significant aortic stenosis is relatively uncommon, affecting about 6 of every 1000 babies born, occurring more often in boys. Aortic stenosis is narrowing of the aortic valve, impeding delivery of blood from the heart to the body. The degree of narrowing is measured as the pressure difference across the aortic valve, which is referred to as the gradient. The higher the gradient, the greater the problem, since the left heart has to work much harder to pump blood to the body. Based on the gradient, aortic stenosis is diagnosed as either trivial, mild, moderate or severe. If the problem is not treated, this overwork causes a thickening of the heart muscle called ventricular hypertrophy.
- What is causing the “click” sound in Lucas’ heart?
- Why is Lucas’ blood pressure lower than normal? Why is his pulse oxygen levels normal?
- What is an electrocardiogram? What was shown on Lucas’ ecg?
- What percentage of babies are born with AVS?
Part IV - Lucas Needs a Procedure
After several days in the I.C.U, Lucas’ vitals are stable, but the blockage in his aorta needs to be repaired. Doctor Brady suggests a minimally invasive procedure called a balloon angioplasty.
Valvar aortic stenosis can be treated surgically or by balloon dilation, a procedure done in the cardiac catheterization lab. During the procedure, catheters (thin plastic tubes) are placed into the large blood vessels in the legs and gently guided to the heart. Because Lucas is so small, Doctor Brady instead suggests they use the umbilical artery. The catheter is threaded through the umbilical artery and into the aorta, following the aorta to where it arches and eventually intersects with the aortic valve.
The catheter tip is placed across the aortic valve and the balloon tip is inflated. The balloon gently dilates the narrowed area. Balloon dilation valvuloplasty can cause valve insufficiency (or leakage), but this is mild in the majority of patients. In approximately 3 percent to 5 percent of the patients the balloon procedure will create severe aortic valve insufficiency. Severe aortic valve insufficiency may require surgical intervention.
With minimal side effects Doctor Brady thinks that this procedure can cause relief of Lucas’s symptoms for several years. The doctor does warn Kelly and Chris that as Lucas grows he may need another procedure to open the valves again, or potentially need a new heart valve.
Lucas remains in the hospital for another week after the valvuloplasty and Doctor Brady confirms that his vital signs have become normal. Lucas is finally allowed to go home!
- Sketch a diagram of the arterial system to show how Lucas’ procedure will be performed, include the heart, aorta, umbilical artery, and the balloon.
- What are some potential complications of the procedure?
- What is “valve insufficiency”? How would doctors determine if Lucas had this problem?
Years Later
Lucas grew up as a normal child, and many of his teachers never even knew he was born with such a major problem with his tiny heart. Lucas would see many cardiologists over the years and is constantly monitored for problems with his heart. Kelly and Chris knew that eventually, they would need to have another surgery.
Recurrent narrowing is perhaps related to patient growth and chronic valve changes. Many of these children will require repeat balloon dilation or surgical valve replacement procedures. When Lucas was 11 years old, his parents received the news they had been dreading: the valve was no longer open enough to provide enough blood flow. They had two options: repeat the balloon dilation valvuloplasty or perform a what is called a Ross Procedure, where the valve is replaced entirely.
At the doctor’s office, Kelly asks for more information about the Ross Procedure. Doctor Brady explains: “In the Ross Procedure, the patient's own pulmonary valve is transplanted to the aortic valve position. The pulmonary valve is then replaced with cadaveric pulmonary valve. In children and young adults, this procedure offers several advantages over traditional aortic valve replacement with manufactured prostheses.”
It was a lot to take in at once. Chris looked troubled. “You mean, you will put a cadaver valve in his heart?” The doctor nodded. Kelly asked another question. “Why wouldn’t you just replace the aortic valve, since it’s the one that has the problem?”
Doctor Brady responded: “That’s a good question, and it has to do with the amount of strain that is on the valves. Artificial and cadaver valves don’t last forever, but ones that are in the pulmonary valve are under less strain and last longer, which means Lucas may be able to go for a long time without needing another surgery.”
Kelly nodded, but Chris did not look convinced. “Why can’t we just do the balloon thing again?”
“It would only be a temporary fix. The valves are calcified and hardened, we could open them with a balloon, but in a few months, they would probably be blocked again. We could also place a mechanical valve in the aorta instead of moving the pulmonary valve. Of course, it’s your choice."
- What are the advantages and disadvantages of both procedures? What would you choose to do?
- Explain why a valve would last longer in the pulmonary position than in the aortic position.
- What would you choose for Lucas given this new information. Defend your position.
- “Patient Choice” is somewhat controversial given then many patients do not have a full understanding of anatomy to make the correct choice. Do you think the doctor should just tell Chris and Kelly what to do, or do you think it is better for patients (or parents of patients) to make the choice? Explain your position.
Case Study Vocabulary - Explain it Like I’m Five (ELI5)
In this case study, you were given many anatomical and medical terms. Summarize, define or describe each of the following in your own words. Don’t just google the words and write a definition, look back in the case and use context clues and your knowledge of anatomy. In fact, do not use dictionary definitions, try to explain the word as if you were trying to put it into terms a 5 year old would understand.
- Arterial Stenosis
- Balloon Dilation
- Cadaveric Pulmonary Valve
- Foramen Ovale
- Cardiologist
- Cyanotic
- Electrocardiogram
- Pulmonary Circulation
- Prosthesis
- Ross Procedure
- Valve Insufficiency
- Ventricular Hypertrophy


