15.1: Introduction
- Page ID
- 122717
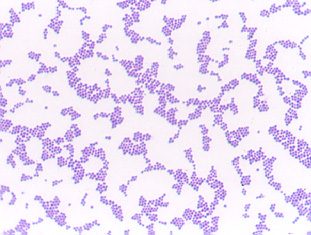
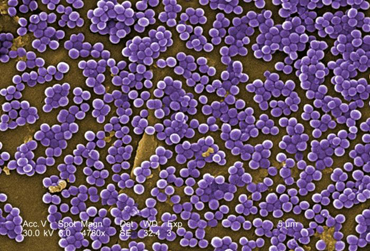
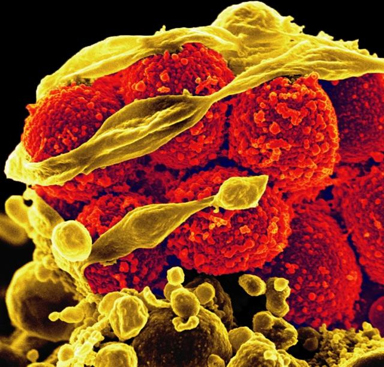
Staphylococci (see Fig. \(\PageIndex{1}\)) are often found in the human nasal cavity (and on other mucous membranes) as well as on the skin. They are Gram-positive cocci 0.5-1.0 µm in diameter and occur singly, in pairs, in short chains, and most commonly, in irregular grape-like clusters. The staphylococci are strongly catalase positive and generally tolerate relatively high concentrations of sodium chloride (7.5-10%). This ability is often employed in preparing media selective for staphylococci. Fig. \(\PageIndex{2}\) shows a scanning electron micrograph of methicillin-resistant Staphylococcus aureus (MRSA), and Fig. \(\PageIndex{3}\) shows an electron micrograph of Staphylococcus aureus (MRSA) destroying an immune cell.
|
Fig. \(\PageIndex{1}\): Gram stain of Staphylococcus aureus |
Fig. \(\PageIndex{2}\): Scanning Electron Micrograph of Methicillin-Resistant Staphylococcus aureus (MRSA) |
Fig. \(\PageIndex{3}\): Scanning Electron Micrograph of Methicillin-Resistant Staphylococcus aureus (red) Killing an Immune Cell (Yellow Cell Debris) |
|---|---|---|
|
|
|
| Note Gram-positive (purple) cocci in clusters | Note staphylococcus arrangement (cocci in irregular, often grape-like clusters). | Note staphylococcus arrangement (cocci in irregular, often grape-like clusters) |
| Copyright; Gary E. Kaiser, Ph.D. The Community College of Baltimore County, Catonsville Campus CC-BY-3.0 | By Content Providers(s): CDC/ Janice Ayers [Public domain]. Courtesy of the Centers for Disease Control and Prevention. | By Content Providers(s): NAID/ Frank Deleo [Public domain]. Courtesy of National Institute of Allergy and Infectious Diseases. |
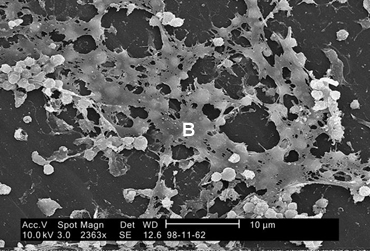
Staphylococcal capsules play a major role in the ability of the bacteria to adhere to and colonize biomaterials.
There are five species of staphylococci commonly associated with clinical infections: Staphylococcus aureus, S. epidermidis, S. haemolyticus, S. hominis and S. saprophyticus.
A. Staphylococcus aureus (coagulase-positive staphylococci)
Staphylococcus aureus is the most pathogenic species and is implicated in a variety of infections. S. aureus is with some frequency found as normal human flora in the anterior nares (nostrils). It can also be found in the throat, axillae, and the inguinal and perineal areas. Approximately 30% of adults and most children are healthy periodic nasopharyngeal carriers of S. aureus. Around 15% of healthy adults are persistent nasopharyngeal carriers. The colonization rates among health care workers, patients on dialysis, and people with diabetes are higher than in the general population.
In the majority of S. aureus infections the source of the organism is either:
- A healthy nasal carrier, or
- Contact with an abscess from an infected individual.
The portal of entry is usually the skin. S. aureus causes pus-filled inflammatory lesions known as abscesses. Depending on the location and extent of tissue involvement, the abscess may be called:
1.Pustules
A pustule is an infected hair follicle where the base of the hair follicle appears red and raised with an accumulation of pus just under the epidermis. Infected hair follicles are also referred to as folliculitis.
2. Furuncles or boils
Furuncles appear as large, raised, pus-filled, painful nodules having an accumulation of dead, necrotic tissue at the base. The bacteria spread from the hair follicle to adjacent subcutaneous tissue.
3. Carbuncles
Carbuncles occur when furuncles coalesce and spread into surrounding subcutaneous and deeper connective tissue. Superficial skin perforates, sloughs off, and discharges pus.
S. aureus also causes impetigo, a superficial blister-like infection of the skin usually occurring on the face and limbs and seen mostly in young children. S. aureus may also cause cellulitis, a diffuse inflammation of connective tissue with severe inflammation of dermal and subcutaneous layers of the skin. S. aureus is also a frequent cause of accidental wound and postoperative wound infections.
Less commonly, S. aureus may escape from the local lesion and spread through the blood to other body areas, causing a variety of systemic infections that may involve every system and organ. Such systemic infections include septicemia, septic arthritis, endocarditis, meningitis, and osteomyelitis, as well as abscesses in the lungs, spleen, liver, and kidneys. S. aureus pneumonia may also be a secondary respiratory complication of viral infections such as measles, and influenza and is a frequent cause of nosocomial pneumonia in patients who are debilitated. Finally, S. aureus is frequently introduced into food by way of abscesses or the nasal cavity of food handlers. If it is allowed to grow and produces an enterotoxin, it can cause staphylococcal food poisoning.
In a 1990-1992 National Nosocomial Infections survey, CDC found S. aureus to be the most common cause of nosocomial pneumonia and operative wound infections, as well as the second most common cause of nosocomial bloodstream infections. Antibiotic resistant S. aureus is a common problem. For example, a survey conducted by CDC reported the proportion of methicillin-resistant isolates S. aureus (MRSA) with sensitivity only to vancomycin increased from 22.8% in 1987 to 56.2% in 1997.
Virulence factors for S. aureus include exotoxins such as leukocidin (kills leukocytes), alpha and delta toxins (damage tissue membranes), microcapsules (resist phagocytic engulfment and destruction), coagulase and protein A (both help resist phagocytic engulfment). Some strains also produce TSST-1 (toxic shock syndrome toxin-1) and cause toxic shock syndrome, usually associated with wounds. Approximately 25% of all S. aureus strains are toxigenic and approximately 6000 gases of toxic shock syndrome occur each year in the U.S. Some strains also produce exfoliatin, an exotoxin that causes scalded skin syndrome, an infection usually seen in infants and young children.
In the past 20 years, both community-associated and hospital-acquired infections with Staphylococcus aureus have increased. This infection rate has been accompanied by a rise in antibiotic-resistant strains - most significantly, methicillin-resistant S. aureus (MRSA) and, more recently, vancomycin-resistant S. aureus.
For further information on virulence factors associated with S. aureus, see the following Softchalk lessons:
- Gram-Positive PAMPs
- The Ability to Adhere to Host Cells
- The Ability to Resist Phagocytic Engulfment
- The Ability to Resist Phagocytic Destruction
- The Ability to Evade Adaptive Immune Defenses
- Type I Toxins
- Type II Toxins that Damage Cell Membranes
- The Ability to Induce Autoimmune Responses
- Type III Toxin
Since most S. aureus strains produce the enzyme coagulase (see the coagulase test described below), they are often referred to as coagulase-positive staphylococci.
Fig. \(\PageIndex{5}\) shows a scanning electron micrograph of Staphylococcus aureus forming a biofilm in an indwelling catheter.
B. Coagulase-Negative Staphylococci
Clinically common species of staphylococci other than S. aureus are often referred to as coagulase-negative staphylococci. These staphylococci are normal flora of the skin and, as such, frequently act as opportunistic pathogens, especially in the compromised host. S. saprophyticus is a relatively common cause of urinary tract infections, especially in healthy young women, but is seldom isolated from other sources. The great majority of infections caused by other coagulase-negative staphylococci, including S. epidermidis, S. haemolyticus, and S. hominis, are associated with intravascular devices (prosthetic heart valves and intra-arterial or intravenous lines) and shunts. Also quite common are infections of prosthetic joints, wound infections, osteomyelitis associated with foreign bodies, and endocarditis.
Although certain reactions may vary from strain to strain, a series of biochemical tests will usually differentiate the most common clinically encountered species of staphylococci. Today we will use several tests to determine if an unknown is S. aureus, S. epidermidis, or S. saprophyticus.
Medscape articles on infections associated with organisms mentioned in this Lab Exercise. Registration to access this website is free.
Contributors and Attributions
Dr. Gary Kaiser (COMMUNITY COLLEGE OF BALTIMORE COUNTY, CATONSVILLE CAMPUS)


