1.16: Cardiovascular Physiology- Heart Rate Responses
- Page ID
- 59161
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\( \newcommand{\dsum}{\displaystyle\sum\limits} \)
\( \newcommand{\dint}{\displaystyle\int\limits} \)
\( \newcommand{\dlim}{\displaystyle\lim\limits} \)
\( \newcommand{\id}{\mathrm{id}}\) \( \newcommand{\Span}{\mathrm{span}}\)
( \newcommand{\kernel}{\mathrm{null}\,}\) \( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\) \( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\) \( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\id}{\mathrm{id}}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\kernel}{\mathrm{null}\,}\)
\( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\)
\( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\)
\( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\) \( \newcommand{\AA}{\unicode[.8,0]{x212B}}\)
\( \newcommand{\vectorA}[1]{\vec{#1}} % arrow\)
\( \newcommand{\vectorAt}[1]{\vec{\text{#1}}} % arrow\)
\( \newcommand{\vectorB}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vectorC}[1]{\textbf{#1}} \)
\( \newcommand{\vectorD}[1]{\overrightarrow{#1}} \)
\( \newcommand{\vectorDt}[1]{\overrightarrow{\text{#1}}} \)
\( \newcommand{\vectE}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash{\mathbf {#1}}}} \)
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\(\newcommand{\longvect}{\overrightarrow}\)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\(\newcommand{\avec}{\mathbf a}\) \(\newcommand{\bvec}{\mathbf b}\) \(\newcommand{\cvec}{\mathbf c}\) \(\newcommand{\dvec}{\mathbf d}\) \(\newcommand{\dtil}{\widetilde{\mathbf d}}\) \(\newcommand{\evec}{\mathbf e}\) \(\newcommand{\fvec}{\mathbf f}\) \(\newcommand{\nvec}{\mathbf n}\) \(\newcommand{\pvec}{\mathbf p}\) \(\newcommand{\qvec}{\mathbf q}\) \(\newcommand{\svec}{\mathbf s}\) \(\newcommand{\tvec}{\mathbf t}\) \(\newcommand{\uvec}{\mathbf u}\) \(\newcommand{\vvec}{\mathbf v}\) \(\newcommand{\wvec}{\mathbf w}\) \(\newcommand{\xvec}{\mathbf x}\) \(\newcommand{\yvec}{\mathbf y}\) \(\newcommand{\zvec}{\mathbf z}\) \(\newcommand{\rvec}{\mathbf r}\) \(\newcommand{\mvec}{\mathbf m}\) \(\newcommand{\zerovec}{\mathbf 0}\) \(\newcommand{\onevec}{\mathbf 1}\) \(\newcommand{\real}{\mathbb R}\) \(\newcommand{\twovec}[2]{\left[\begin{array}{r}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\ctwovec}[2]{\left[\begin{array}{c}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\threevec}[3]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\cthreevec}[3]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\fourvec}[4]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\cfourvec}[4]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\fivevec}[5]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\cfivevec}[5]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\mattwo}[4]{\left[\begin{array}{rr}#1 \amp #2 \\ #3 \amp #4 \\ \end{array}\right]}\) \(\newcommand{\laspan}[1]{\text{Span}\{#1\}}\) \(\newcommand{\bcal}{\cal B}\) \(\newcommand{\ccal}{\cal C}\) \(\newcommand{\scal}{\cal S}\) \(\newcommand{\wcal}{\cal W}\) \(\newcommand{\ecal}{\cal E}\) \(\newcommand{\coords}[2]{\left\{#1\right\}_{#2}}\) \(\newcommand{\gray}[1]{\color{gray}{#1}}\) \(\newcommand{\lgray}[1]{\color{lightgray}{#1}}\) \(\newcommand{\rank}{\operatorname{rank}}\) \(\newcommand{\row}{\text{Row}}\) \(\newcommand{\col}{\text{Col}}\) \(\renewcommand{\row}{\text{Row}}\) \(\newcommand{\nul}{\text{Nul}}\) \(\newcommand{\var}{\text{Var}}\) \(\newcommand{\corr}{\text{corr}}\) \(\newcommand{\len}[1]{\left|#1\right|}\) \(\newcommand{\bbar}{\overline{\bvec}}\) \(\newcommand{\bhat}{\widehat{\bvec}}\) \(\newcommand{\bperp}{\bvec^\perp}\) \(\newcommand{\xhat}{\widehat{\xvec}}\) \(\newcommand{\vhat}{\widehat{\vvec}}\) \(\newcommand{\uhat}{\widehat{\uvec}}\) \(\newcommand{\what}{\widehat{\wvec}}\) \(\newcommand{\Sighat}{\widehat{\Sigma}}\) \(\newcommand{\lt}{<}\) \(\newcommand{\gt}{>}\) \(\newcommand{\amp}{&}\) \(\definecolor{fillinmathshade}{gray}{0.9}\)Objectives:
At the end of the lab you will be able to…
1. Be able to associate observed changes in rate, rhythm of the heart along with changes in cardiac functions associated with altered fluid flow from changes in body position, thoracic volumes (impact breathing has on amount of volume heart can achieve) and physical exertion.
2. Be able to explain how modifiable and non-modifiable factors impact the observed changes.
3. Understand the issue of norms within a population and the factors of associative analysis.
Pre-Lab
1. What factors will change heart rate?
2. What is the relationship between the volume of blood returning to the heart and the volume of blood that can be ejected from the heart?
3. Why does fluid pressure change when someone goes from supine to standing?
4. What is the principal reason that heart rate will change during exercise?
5. Develop your hypothesis.
I. INTRODUCTION
Examination of heart function and cardiac cycles allows you to compare the electrical output of the heart to the morphological changes associated with the movement of blood through the chambers of the heart. These changes reflect the fluid movement throughout the blood vessels of body and are influenced by the level of resistance to flow through the vessels. This pattern of activity and the timing of mechanical events under normal conditionals last approximately 600 msec from the depolarization of the SA node through the contraction within the ventricular systole. A contraction pattern that is then be followed by a period of limited electrical activity as the heart is deemed to be in the intercycle refractory period that allows for venous return to the heart (finalized atrial diastole) and thus allow for complete venous return and “filling” of the heart. Each full cycle of the heart from the resting “fill” through the contraction of the ventricles and ejection of blood into the arteries of the body is deemed a heartbeat or one cardiac cycle occurring every 900 msec to 1.2 seconds for adults. The cadence that the heart uses over time is thus referenced as heart rate. The means by which the cycle is regulated and modulated is based on several physiological and anatomical factors. These factors include the volume of blood being moved, the resistance to blood leaving the heart (i.e. blood pressure), and the relative amount of autonomic nervous stimulus at the SA node and throughout the heart. All of these factors will impact how a contraction will take place and the effectiveness of the contraction. In which we know that as volume of load increases, the strength of contraction will increase, and this will generate a greater amount of blood being moved. Whereas as resistance to flow increases (more total peripheral resistance) a larger contraction is necessary to move a smaller volume.
Peripheral Resistance and Impact on “Blood” Pressures:
The flow of blood through the blood vessels (arteries and veins) is explained by the physics of fluid flow through a tube. In the case of the vessels, the tubes will offer varying degrees of resistance to flow and force upon the fluid within the blood vessels as blood moves through them. All in all, there are three factors that ultimately determine the resistance to flow and total pressure within the vessels of the cardiovascular system: vessel diameter, blood viscosity (how well it can flow/or not flow) and the total amount of vessel that fluid is having to move through to get around the system, see Haigen-Pousalt equation. These factors contribute to establishing a fluid pressure that the blood exerts onto the vessels, i.e. blood pressure. Typically, this pressure is discussed in relationship to the pulses of blood ejecting from the heart during ventricular systole (systolic pressure) and diastole (diastolic pressure). The combination of fluid pressure with anatomical changes (referred to as compliance) in the vessels establish a resistance of flow that impacts the propulsion of blood through the arteries, and veins, throughout the circuit of the vessels within the body and ultimately impacts the pressures measured clinically.
Haigen-Pousalt Equation: 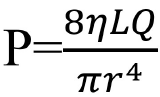 ; where P is pressure within the vessel, L is length of vessel, Q is volume of flow through vessel, r is radius of the vessel and η is the viscosity (resistance to flow) of the fluid.
; where P is pressure within the vessel, L is length of vessel, Q is volume of flow through vessel, r is radius of the vessel and η is the viscosity (resistance to flow) of the fluid.
|
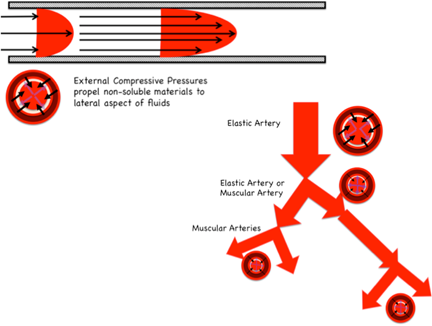
Figure 1. Combination of the compressive force of tunica media and the branching of arteries leading to a change in the external compressive force and resulting internal blood pressures within the lumen. |
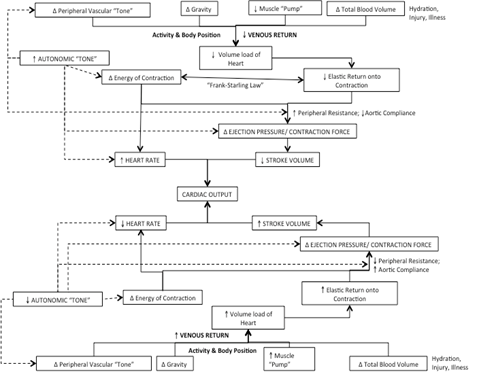
Due to anatomical and physiological differences, the amount of pressure within vessels will vary. As such, arteries exert a higher resistance to flow than veins due to the constant tension of the tunica media which means that the pressures will be higher in the blood while on the arterial side of flow and lessens to near zero as the fluid moves through the venal side of flow. The pressure within the lumen of the artery is controlled and regulated by the muscles and elastic connective tissue within the tunica media that when compliant will generate an inward force, pressing onto the fluid within the vessel (a positive pressure). This positive pressure thus propels the fluid forward when there is no propulsive force of the pulse of blood being ejected from the heart, figure 1. As fluid moves through the arteries the amount of propulsive force from the ventricle diminishes (from the highest pressure at the aortic valve) and the only forward pressure that is imparted on the fluid will come from the positive pressure of the vessel lumen. This drop in propulsive force is accompanied by an increase in the length of lumen (due to the branching of the arteries) and reduction in volume within the lumen that results in the phenomenon of gradual decrease of blood pressure as blood moves through the branching network of vessels. Additionally, this pressure will vary based the diameter of the vessel and the ability to be compliant to meet the change in fluid pressures as volume shifts with each pulse of blood ejecting from the heart. Ultimately this relationship between the ability for the lumen to adjust to the pressure with the lumen develops resistance to flow where any increase in compliance leads to a reduction in pressure, while and decrease in compliance leads to an increase in blood pressure and indicates the functionality of the vessels. An issue we see with individuals in normal compensatory responses to everyday stresses and can be witnessed regarding issues of compliance and tension responses to orthostatic challenges, e.g., individuals when moving rapidly from a lying to a standing position; or in response to exercise at very high levels of exertion; or even within ventilation, as increased lung volume and/or intra-abdominal pressures restrict volume compliance within the arteries of the thorax. Regardless of the reason, any excessive pressure changes lead to a feedback loop that triggers a baroreceptive reflex, an alteration of systemic peripheral resistance and a resulting change in heart rate to accommodate for an alteration in stroke volume, figure 2.
Norms and Variability in Measures:
The cardiac cycle (Heart Rate, HR) is influenced by several factors that relate to the homeostatic regulation of cardiac output, the determination of volume of blood moved per minute based on the product of heart rate, HR (beats/min) and stroke volume, SV (mL/beat). The values for individuals are highly variable based on everything from body position, to ventilation (figure 2), to factors such as age, gender, and several health and fitness factors (principally controlled by the amount of activity) that change the rate and volume of venous return that directly impacts the amount of blood circulated per cardiac cycle. Most of this modification is based on the concept known as the Frank-Starling Law, which indicates the relationship between venous return (VR) with end systolic volume (ESV), end diastolic volume (EDV), stroke volume (SV), and thus heart rate (HR) and ejection fraction (EF). Simply stated, the Frank-Starling Law (i.e. length-tension relationship) of cardiac function indicates that a slower HR allows for increased filling of both atrium and ventricle and thus provides for an increase in EDV and SV as well provides a stronger contraction of the cardiac muscle.
|
Figure 2. Flow-chart detailing the effects of the changes of venous return leading changes in stroke volume and heart rates |
Thus, there is a direct relationship between VR with SV (i.e. increase in VR leads to a proportional increase in SV) and an inverse relationship with HR (i.e. increase in VR leads to a proportional decrease in HR) and vice versa when VR diminishes, as seen with physical activity, changes in body position, or the simple action of ventilation. The relationship when seen in response to any type of activity leads to the compensatory response of changes in HR, or a cardiac drift. The degree of drift is dependent on adaptions that occur within the cardiovascular system to repeated bouts of activity. In which improved arterial compliance and greater pressure reservoirs that generates greater venous return leading to an increased SV thus a lowering HR and improved cardiovascular function both acutely (during the activity) as well as chronically (due to adaptations) regardless of the type of physical activity that is employed for training and creates improvements in EF as SV increases and EDV decreases within each cardiac cycle. Thus, it would be expected that those who are more active would have lower HR and pressures than those who are less active.
Acutely, this relationship can be exhibited through a response of cardiac shift inducing cardiac drift. A rapid change in VR is typically associated with a systemic hypotensive response (i.e. rapid drop in peripheral resistance/blood pressure) that is accompanied by a rapid drop in SV and a rapid increase in HR, referred to a baroreceptive reflex. Additionally, there is a neural and neuroendocrine modification that is associated with the concept of autonomic tone, primarily because of epinephrine and norepinephrine have on a tissues ability to depolarize any increased exposure to either chemical increases the likelihood for depolarization at the SA node and along the conductive pathways, along with the rate of force development within the contractile tissues of the myocardium of the heart. Thus, combining to increase the rate of cardiac cycles. Antagonistically, exposure to acetylcholine reduces the rate of depolarization at the SA node and along the conductive pathway thus reducing the rate of depolarization waves and the associated frequency of the cardiac cycles. As such, we must indicate the type of measurement being obtained and referenced. The most common references are the non-exertional (HRnon-exertion=HR when not actively involved in physical activity) with a normal for intrinsic rate of 72-92 bpm (range from 45-140 bpm), resting (HRrest= HR at complete rest without external/internal stressor, i.e. supine in quite dark room after at least 15-minutes following initiation of the test). There is sometimes confusion between the idea of “resting” and “non-exertional” HR, but these are two separate measures based on the testing conditions under which the cardiac cycles are being sampled. Additionally there are the for measurements for exertion or physical activity such as: minimal exertion (HRmin=HR at minimal exertion, but always given in relation to the maximal exertion for the person); maximal exertion (HRmax=maximal sustainable HR (based on 180-second of stable response), related to maximal exertion or maximal oxygen consumption, VO2max, and typically obtained with a stress test or test of aerobic fitness); age-predicted maximal (HRAPM= age-predicted maximal HR based on the equation of HRAPM=220-age or HRAPM=208-.8*age (in whole yr.)); and the reserve to maximal (HRreserve= percentage of difference between HRmax (or HRAPM) and HRmin that is then added to the HRnon-exertion, is usually used in order to determine HR range for training or rehabilitative purpose).
References:
Brooks GA, Fahey TD, Baldwin KM. 2005.Ch. 15 Circulation and Its Control and Ch. 16 Cardiovascular Dynamics During Exercise, from Exercise Physiology, Human Bioenergetics and Its Application, 4th Ed. p.312-334, 340-359. McGraw-Hill.
Dampney RAL, Coleman MJ, Fontes MAP, Hirooka Y, Horiuchi J, Polson JW, Potts PD, Tagawa T. 2003. Central mechanisms underlying short-term and long-term regulation of the cardiovascular system. Proceedings of the Australian Physiology and Pharmacological Society 32(1), 119-135.
Evans RG, Ventura S, Dampney RAL, Ludbrook. 2003. Neural mechanisms in the cardiovascular responses to acute central hypovolaemia. Proceedings of the Australian Physiology and Pharmacological Society 32(1), 1-12.
Keener J, Sneyd J. 2009. Ch. 11 Circulatory System, Ch. 12 The Heart, from Antman SS, Marsden JE, Sirovich L (editors) Mathematical Physiology II: Systems Physiology, 2nd Ed. p. 471-522, 523-626. Springer-Vertang
Kingwell BA. 2003. Large artery stiffness: Implications for exercise capacity and cardiovascular risk. Proceedings of the Australian Physiology and Pharmacological Society 32(1), 156-161.
Mammen BA. 1995. Ch5.Basic Electrocardiogram, from Irwin S, Tecklin JS (editors) Cardiopulmonary Physical Therapy 3rd Ed. p.48-75. Mosby
Rowell, LB. 1974. Human cardiovascular adjustments to exercise and thermal stress. Physiol Rev. 54 (1) 75-159.
Terjung RL, Mathien GM, Erney TP, Ogilive RW. 1988 Peripheral adaptations to low blood flow in muscles during exercise. Am J Cardiol 62(8); 15E-19E
Purpose:
Therefore, the purpose of this experiment is to examine the differences in heart rates and changes to a non-exertional situations, so as to compare differences between individuals based on modifiable and non-modifiable factors known to impact heart functions.
Hypothesis:
EXPERIMENTAL OBJECTIVES
At the end of the experiment students should
1) Be able to use a stethoscope to correctly auscultate sounds for distinct Korsakoff sounds to measure blood pressure.
MATERIALS
- Heart Rate Monitor
- Steps and Risers
- Stop-watch/timer
METHODS
1. Place the heart rate monitor on the test subject, you need to place it so that it can read whenever you obtain a pulse count
2. Have your subject move from the seated position on to the floor in front of your lab station and lay down in the supine position. Ensure that head, shoulders, and torso are supported and that lower extremities are not extended at the knee (ask subject to slightly bend at the knee and place feet flat on the floor).
a. If subject needs to reposition, allow them to do so, but encourage them to remain in a supine position with head and neck completely supported.
b. Wait 60 seconds before starting the tests
3. Testing Heart Rate Responses
a. Supine Test
i. Make sure your subject is in the most comfortable position
1. Ensure that your subject is breathing normally without large inhalations/exhalations and minimal to no movement.
ii. After 30-seconds in the supine position, obtain the pulse rate by reading the heart rate monitor by watching the monitor (without your test subject moving) for 15-seconds
1. Record the reading at the end of the 15-seconds
b. Supine-to-Stand-to-Sit
i. With your test subject still in the supine position, take a lab chair and place it next to the test subject
ii. Now give a countdown, “3…2…1…stand” have your subject stand-up as quickly as possible and then sit on the chair provided.
iii. Immediately upon sitting check the heart rate monitor and continue to check the monitor as they sit down. Record heart rate at the end of the transition in “Change of Position”
1. Ensure that your test subject safely sits on the chair provided and is breathing normally without large inhalations/exhalations for 60-seconds
c. Ventilation Test
i. With your test subject seated comfortably, instruct them that for the next segment of the experiment they will change their inhalation/exhalation pattern based on verbal cues to “Breathe deeply and slowly, and then hold their breath until told to exhale.” Use the example of taking breaths for the doctor during an examination and to only breathe when instructed.
ii. Have your subject practice this breathing cycle through 3-ventilation cycles so that both of you are comfortable with the test
iii. Wait 30-seconds and watch the heart rate monitor, instruct the test subject to inhale as deeply as possible
i. Obtain the pulse rate at the end of inhalation but before you have them exhale
ii. Repeat 3 times, average HR obtained, record data in data table for “Inhale”
a. Now repat the breathing exercise but instead of recording the heart for inhaling you will record exhalation
i. Record data in data table for “Exhale”
d. Valsalva test
i. Obtain the pulse rate by reading the heart rate monitor, record data in data table “Pre-Valsalva”
ii. Have the test subject place themselves into a comfortable seated position with their back fully supported in the chair. Once ready, indicate that you are performing the Valsalva test as instructed the test subject to breath on the cue
1. Tell your subject that they are going to take a very deep breath and then will held the breath. While holding the breath tell them that you will ask them to squeeze their abdomen, press their tongue into the hard palate of their mouth, and hold the contraction for 25-seconds.
2. Make sure that you can view the heart rate monitor while also keeping the test subject directly in your line of sight for safety. Give them a countdown and then have the subject hold their breath while squeezing their abdomen and pressing the tongue into the hard palate of the mouth.
3. At 15-seconds into the hold:
a. Obtain the pulse rate by reading the heart rate monitor for 5-seconds, record data in data table “Valsalva”
4. As soon as 25 seconds have elapsed, have your subject relax and begin breathing normally for 5-seconds at 5-seconds, obtain a pulse rate from the heart rate monitor and record in “Post-Valsalva”
e. Response to Brief Physical Exertion
i. Clear the area in front of the seated position place an aerobic step with 1-2 risers under the top (approximately 6-8 inches).
ii. Have the test subject face the step and place their right foot on top of the step with left foot on the ground.
1. With the test subject standing facing the steps, obtain the pulse rate by reading the heart monitor and record data in data table “Pre-Exertion”
iii. Have the test subject exert themselves by using the following cadence have the subject stride onto the step continuously for 60-seconds at a pace they can comfortably keep without pause or termination of striding, stepping up on the right foot every second:
1. Right foot on step; stride forward with left foot and place left foot on top of step.
2. On contact of left foot, transfer weight to left limb and stride right foot to floor (move limb backwards) once in contact with floor (but without stopping) stride forward with right foot and place right foot on top of step.
3. On contact of right foot, transfer weight to right limb and stride left foot to floor (move limb backwards) once in contact with floor (but without stopping) stride forward with left foot and place left foot on top of step repeating the initial movement.
4. Continue without stopping for 60-seconds.
5. At the 60-second mark of exercise, check the heart rate monitor and then give the subject a countdown of “3…2...1…stop”
6. Record the heart rate obtained immediately at the end of exercise in “Post-Exertion”
iv. Have the subject will stop stepping and stand in place on the floor without excessive movement for 20-seconds. During this time keep watch of the test subject to ensure that they are safe following the exertion. After 20-seconds, have your subject sit comfortably in their chair
**Make sure to upload results to Google Document for use in lab report**
RESULTS:
Designation of Level of Physical Activity: (based on average weekly activity level over the last 3 months only)
Low: Less than 3 days of activity at moderate intensity for at least 30-minutes
Moderate: Between 3 and 5 days of activity at moderate intensity for at least 30-minutes
High: More than 5 days of activity at moderate intensity for at least 30-minutes
Demographics Subject 1
Gender:
Age:
Subject is classified as:
Days per week physically active:
Demographics Subject 2
Gender:
Age:
Subject is classified as:
Days per week physically active:
Table 3. Table of heart rate (BPM) responses for each of the testing conditions based on the individual test subject within each of the testing scenarios.
|
|
Supine |
Change of Position |
Inhale |
Exhale |
Pre-Valsalva |
Valsalva |
Post-Valsalva |
Pre-Exertion |
Post-Exertion |
|
Subject #1 |
|
|
|
|
|
|
|
|
|
|
Subject #2 |
|
|
|
|
|
|
|
|
|
Upload your results to the group data table for analysis
Table 4. Change in heart rate (bpm) from the supine position based on each of the testing scenarios.
Calculations are always Condition-Supine for each of the measurements
|
|
Change of Position |
Inhale |
Exhale |
Pre-Valsalva |
Valsalva |
Post-Valsalva |
Pre-Exertion |
Post-Exertion |
|
Subject #1 |
|
|
|
|
|
|
|
|
|
Subject #2 |
|
|
|
|
|
|
|
|
For lab report, provide graph of responses based on relationship of heart rate (measured variable) with condition deemed to be manipulated variable
Discussion: In 2-to-3 coherent paragraphs discuss your findings based on your test subjects and the class averages based on the demographic identifiers and your understanding of the regulation of the cardiac cycle. Make sure to explain the reason for the change. (In this discussion think about (do not answer questions as individual assessment questions, use to help formulate your interpretation of the data): comparison of kinematics between testing situation and the responses within each of the groups based on demographics and factors that influence heart functions. What impact does body posture, changes to intrathoracic pressures, changes due to exertion, impact of gender and level of activity (Why is activity given based on a “high”, “moderate”, or “low” identifier?) have on responses seen? Make sure that you’re attempting to explain the WHY and the HOW of the WHAT {give #’s} occurred. What do changes in sounds of the heart indicate is occurring? How do the changes in heart rates correlate with changes in the pressures that would be experienced in the vessels and the volume of blood returning to the heart?)