12.7: Pancreas
- Page ID
- 17097
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\( \newcommand{\dsum}{\displaystyle\sum\limits} \)
\( \newcommand{\dint}{\displaystyle\int\limits} \)
\( \newcommand{\dlim}{\displaystyle\lim\limits} \)
\( \newcommand{\id}{\mathrm{id}}\) \( \newcommand{\Span}{\mathrm{span}}\)
( \newcommand{\kernel}{\mathrm{null}\,}\) \( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\) \( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\) \( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\id}{\mathrm{id}}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\kernel}{\mathrm{null}\,}\)
\( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\)
\( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\)
\( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\) \( \newcommand{\AA}{\unicode[.8,0]{x212B}}\)
\( \newcommand{\vectorA}[1]{\vec{#1}} % arrow\)
\( \newcommand{\vectorAt}[1]{\vec{\text{#1}}} % arrow\)
\( \newcommand{\vectorB}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vectorC}[1]{\textbf{#1}} \)
\( \newcommand{\vectorD}[1]{\overrightarrow{#1}} \)
\( \newcommand{\vectorDt}[1]{\overrightarrow{\text{#1}}} \)
\( \newcommand{\vectE}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash{\mathbf {#1}}}} \)
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\(\newcommand{\longvect}{\overrightarrow}\)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\(\newcommand{\avec}{\mathbf a}\) \(\newcommand{\bvec}{\mathbf b}\) \(\newcommand{\cvec}{\mathbf c}\) \(\newcommand{\dvec}{\mathbf d}\) \(\newcommand{\dtil}{\widetilde{\mathbf d}}\) \(\newcommand{\evec}{\mathbf e}\) \(\newcommand{\fvec}{\mathbf f}\) \(\newcommand{\nvec}{\mathbf n}\) \(\newcommand{\pvec}{\mathbf p}\) \(\newcommand{\qvec}{\mathbf q}\) \(\newcommand{\svec}{\mathbf s}\) \(\newcommand{\tvec}{\mathbf t}\) \(\newcommand{\uvec}{\mathbf u}\) \(\newcommand{\vvec}{\mathbf v}\) \(\newcommand{\wvec}{\mathbf w}\) \(\newcommand{\xvec}{\mathbf x}\) \(\newcommand{\yvec}{\mathbf y}\) \(\newcommand{\zvec}{\mathbf z}\) \(\newcommand{\rvec}{\mathbf r}\) \(\newcommand{\mvec}{\mathbf m}\) \(\newcommand{\zerovec}{\mathbf 0}\) \(\newcommand{\onevec}{\mathbf 1}\) \(\newcommand{\real}{\mathbb R}\) \(\newcommand{\twovec}[2]{\left[\begin{array}{r}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\ctwovec}[2]{\left[\begin{array}{c}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\threevec}[3]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\cthreevec}[3]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\fourvec}[4]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\cfourvec}[4]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\fivevec}[5]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\cfivevec}[5]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\mattwo}[4]{\left[\begin{array}{rr}#1 \amp #2 \\ #3 \amp #4 \\ \end{array}\right]}\) \(\newcommand{\laspan}[1]{\text{Span}\{#1\}}\) \(\newcommand{\bcal}{\cal B}\) \(\newcommand{\ccal}{\cal C}\) \(\newcommand{\scal}{\cal S}\) \(\newcommand{\wcal}{\cal W}\) \(\newcommand{\ecal}{\cal E}\) \(\newcommand{\coords}[2]{\left\{#1\right\}_{#2}}\) \(\newcommand{\gray}[1]{\color{gray}{#1}}\) \(\newcommand{\lgray}[1]{\color{lightgray}{#1}}\) \(\newcommand{\rank}{\operatorname{rank}}\) \(\newcommand{\row}{\text{Row}}\) \(\newcommand{\col}{\text{Col}}\) \(\renewcommand{\row}{\text{Row}}\) \(\newcommand{\nul}{\text{Nul}}\) \(\newcommand{\var}{\text{Var}}\) \(\newcommand{\corr}{\text{corr}}\) \(\newcommand{\len}[1]{\left|#1\right|}\) \(\newcommand{\bbar}{\overline{\bvec}}\) \(\newcommand{\bhat}{\widehat{\bvec}}\) \(\newcommand{\bperp}{\bvec^\perp}\) \(\newcommand{\xhat}{\widehat{\xvec}}\) \(\newcommand{\vhat}{\widehat{\vvec}}\) \(\newcommand{\uhat}{\widehat{\uvec}}\) \(\newcommand{\what}{\widehat{\wvec}}\) \(\newcommand{\Sighat}{\widehat{\Sigma}}\) \(\newcommand{\lt}{<}\) \(\newcommand{\gt}{>}\) \(\newcommand{\amp}{&}\) \(\definecolor{fillinmathshade}{gray}{0.9}\)Giving yourself an injection can be difficult, but for someone with diabetes, it may be a matter of life or death. The person in the photo has diabetes and is injecting himself with insulin, the hormone that helps control the level of glucose in the blood. Insulin is produced by the pancreas.
Introduction to the Pancreas
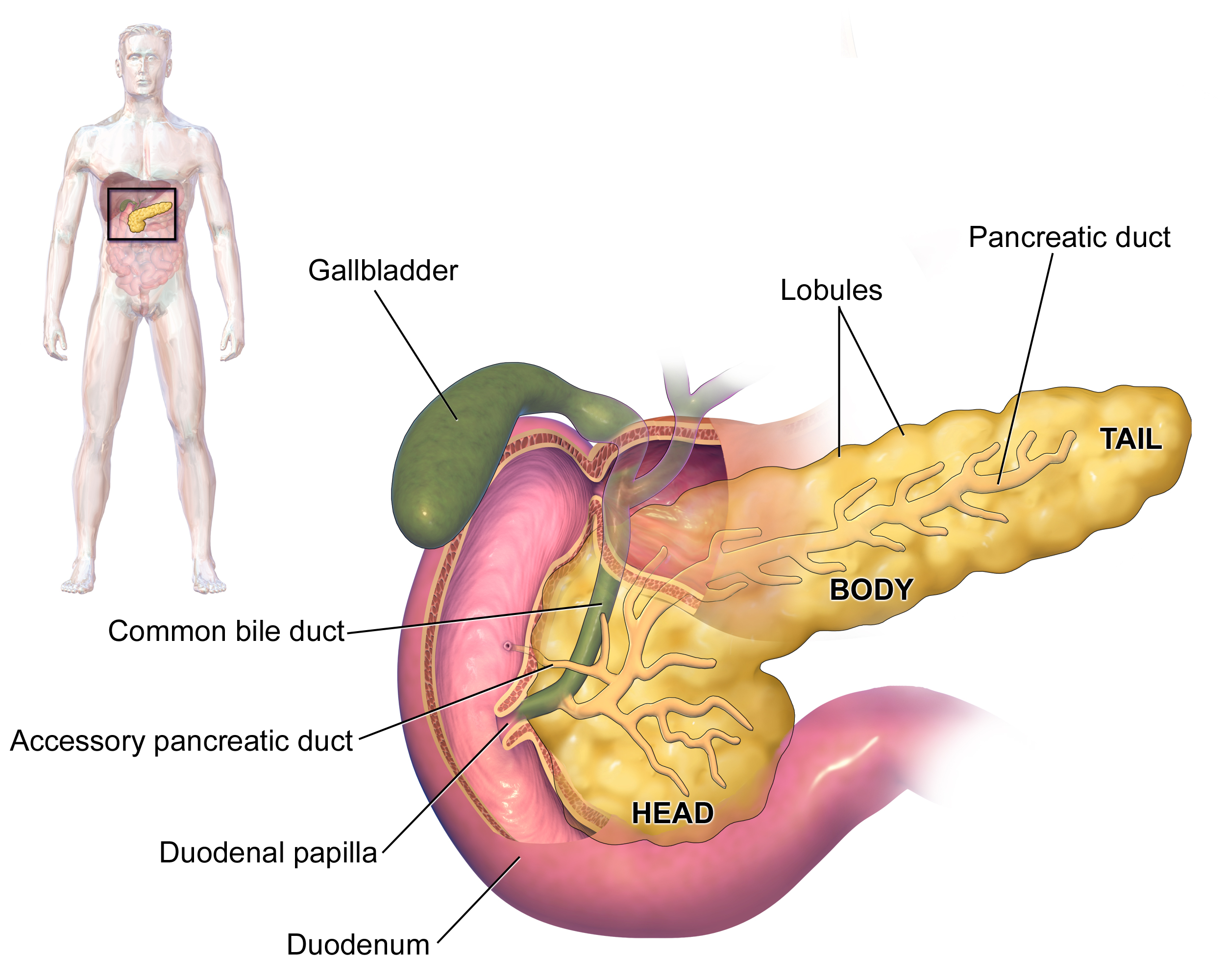
The pancreas is a large gland located in the upper left abdomen behind the stomach, as shown in the figure below. The pancreas is about 15 centimeters (6 in.) long; and it has a flat, oblong shape. Structurally, the pancreas is divided into a head, body, and tail. Functionally, the pancreas serves as both an endocrine gland and an exocrine gland.
- As an endocrine gland, the pancreas is part of the endocrine system. As such, it releases hormones, such as insulin, directly into the bloodstream for transport to cells throughout the body.
- As an exocrine gland, the pancreas is part of the digestive system. As such, it releases digestive enzymes into ducts that carry the enzymes to the gastrointestinal tract where they assist with digestion. In this concept, the focus is on the pancreas as an endocrine gland. You can read about the pancreas as an exocrine gland in the chapter Digestive System.
The Pancreas as an Endocrine Gland
The tissues within the pancreas that have an endocrine role exist as clusters of cells called pancreatic islets. They are also called the islets of Langerhans. In Figure \(\PageIndex{3}\), you can see pancreatic tissue, including islets. There are approximately 3 million pancreatic islets, and they are crisscrossed by a dense network of capillaries. The capillaries are lined by layers of islet cells that have direct contact with the blood vessels, into which they secrete their endocrine hormones.
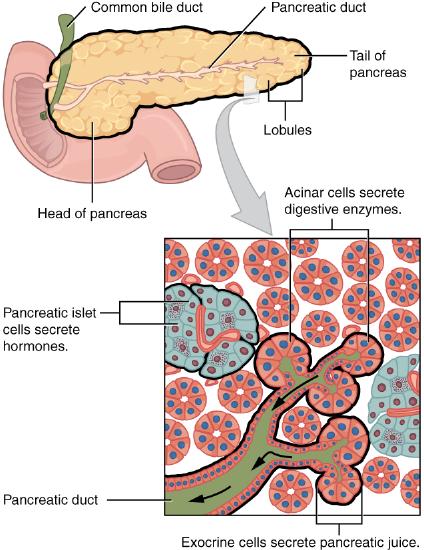
The pancreatic islets consist of four main types of cells, each of which secretes a different endocrine hormone. However, all of the hormones produced by the pancreatic islets play crucial roles in glucose metabolism and the regulation of blood glucose levels, among other functions.
- Islet cells called alpha (α) cells secrete the hormone glucagon. The function of glucagon is to increase the level of glucose in the blood. It does this by stimulating the liver to convert stored glycogen into glucose, which is released into the bloodstream.
- Islet cells called beta (β) cells secrete the hormone insulin. The function of insulin is to decrease the level of glucose in the blood. It does this by promoting the absorption of glucose from the blood into fat, liver, and skeletal muscle cells. In these tissues, the absorbed glucose is converted into glycogen, fats (triglycerides), or both.
- Islet cells called delta (δ) cells secrete the hormone somatostatin. This hormone is also called the growth hormone inhibiting hormone because it inhibits the anterior lobe of the pituitary gland from producing growth hormone. Somatostatin also inhibits the secretion of pancreatic endocrine hormones and pancreatic exocrine enzymes.
- Islet cells called gamma (γ) cells secrete the hormone pancreatic polypeptide. The function of pancreatic polypeptide is to help regulate the secretion of both endocrine and exocrine substances by the pancreas.
Disorders of the Pancreas
There are a variety of disorders that affect the pancreas. They include pancreatitis, pancreatic cancer, and diabetes mellitus.
Pancreatitis
Pancreatitis is inflammation of the pancreas. It has a variety of possible causes including gallstones, chronic alcohol use, infections such as measles or mumps, genetic causes, and certain medications. Pancreatitis occurs when digestive enzymes produced by the pancreas damage the gland’s tissues, which causes problems with fat digestion. The disorder is usually associated with intense pain in the central abdomen, and the pain may radiate to the back. Yellowing of the skin and whites of the eyes (Figure \(\PageIndex{4}\)), which is called jaundice, is a common sign of pancreatitis. People with pancreatitis may also have pale stools and dark urine. Treatment of pancreatitis includes administering drugs to manage pain and addressing the underlying cause of the disease, for example, by removing gallstones.

Pancreatic Cancer
There are several different types of pancreatic cancer that may affect either the endocrine or the exocrine tissues of the gland. Cancers affecting the endocrine tissues are all relatively rare. However, their incidence has been rising sharply. It is unclear to what extent this reflects increased detection, especially through medical imaging techniques. Unfortunately, pancreatic cancer is usually diagnosed at a relatively late stage when it is too late for surgery, which is the only way to cure the disorder. In the United States, pancreatic cancer is the fourth most common cause of death due to cancer.
Pancreatic cancer is rare before the age of 40 and occurs most often after the age of 60. Factors that increase the risk of developing pancreatic cancer include smoking, chronic pancreatitis, and diabetes. About one in four cases of pancreatic cancer are attributable to smoking. Certain rare genetic conditions are also risk factors for pancreatic cancer.
Diabetes Mellitus
By far the most common type of pancreatic disorder is diabetes mellitus, more commonly called simply diabetes. There are many different types of diabetes, but diabetes mellitus is the most common. It occurs in two major types, type 1 diabetes and type 2 diabetes. The two types have different causes and may also have different treatments, but they generally produce the same initial symptoms, which include excessive urination and thirst. These symptoms occur because the kidneys excrete more urine in an attempt to rid the blood of excess glucose, and loss of water in urine stimulates greater thirst. Other signs and symptoms of diabetes are listed in Figure \(\PageIndex{5}\).
When diabetes is not well controlled, it is likely to have several serious long-term consequences. Most of these consequences are due to damage to small blood vessels because of high blood levels of glucose. Damage to blood vessels, in turn, may lead to an increased risk of coronary artery disease and stroke. Damage to blood vessels in the retina of the eye can result in gradual vision loss and blindness. Damage to blood vessels in the kidneys can lead to chronic kidney disease, sometimes requiring dialysis or a kidney transplant. Long-term consequences of diabetes may also include damage to the nerves of the body, known as diabetic neuropathy. In fact, this is the most common complication of diabetes. Symptoms of diabetic neuropathy may include numbness, tingling, and pain in the extremities.
Type 1 Diabetes
Type 1 diabetes is a chronic autoimmune disorder in which the immune system attacks the insulin-secreting beta cells of the pancreas. As a result, people with type 1 diabetes lack the insulin needed to keep blood glucose levels within the normal range. Type 1 diabetes may develop in people of any age but is most often diagnosed before adulthood. For type 1 diabetics, insulin injections are critical for survival.
Type 2 Diabetes
Type 2 diabetes is the single most common form of diabetes. The cause of high blood glucose in this form of diabetes usually includes a combination of insulin resistance and impaired insulin secretion. Both genetic and environmental factors play roles in the development of type 2 diabetes. Management of type 2 diabetes includes changes in diet and physical activity, which may increase insulin sensitivity and help reduce blood glucose levels to normal ranges. Medications may also be used as part of the treatment, as may insulin injections.
Some patients with type 1 diabetes have been given pancreatic islet cells transplants from other human donors. If the transplanted cells are not rejected by the recipient’s immune system, they can cure the patient of diabetes. However, only about 1,000 such surgeries have been performed over the past 10 years because of a shortage of appropriate human donors.
In June of 2016, a research team led by Dr. David K.C. Cooper at the Thomas E. Starzl Transplantation Institute in Pittsburgh, Pennsylvania, reported on their work developing pig islet cells for transplant into human diabetes patients. The researchers genetically engineered the pig islet cells to be protected from the human immune response. As a result, patients receiving transplanted cells would require only minimal suppression of their immune system after the surgery. The pig islet cells would also be less likely to transmit pathogenic agents because the animals could be raised in a controlled environment.
The researchers have successfully transplanted the pig islet cells into monkey models of type 1 diabetes. As of June 2016, the scientists were looking for funding to undertake clinical trials in humans with type 1 diabetes. Dr. Cooper predicted then that if the human trials go as well as expected, the pig islet cells could be available for curing patients in as little as two years.
Review
- Describe the structure and location of the pancreas.
- Distinguish between the endocrine and exocrine functions of the pancreas.
- Identify the four types of pancreatic islet cells and the endocrine hormone each type of cell produces.
- What is pancreatitis? What are the possible causes and effects of pancreatitis?
- Describe the incidence, prognosis, and risk factors of cancer of the endocrine tissues of the pancreas.
- Compare and contrast type 1 and type 2 diabetes.
- If the alpha islet cells of the pancreas were damaged to the point that they no longer functioned, how would this affect blood glucose levels? Would the administration of insulin be more likely to help or hurt the condition? Explain your answer.
- Explain how the pancreas is able to regulate the production of its own endocrine hormones, to some extent.
- True or False. The pancreas is part of both the digestive system and the endocrine system.
- Give an example of how the pancreas can regulate the production of hormones from the pituitary gland.
- Which is the most common form of diabetes mellitus?
- Explain why diabetes causes excessive thirst.
- Damage to __________ is the underlying cause of many of the long-term consequences of diabetes.
- the adrenal gland
- gamma islet cells
- blood vessels
- the pituitary gland
Explore More
Attributions:
- Insulin Application by Mr. Hyde, public domain, via Czech Wikipedia
- Pancreas anatomy by Blausen.com staff (2014). "Medical gallery of Blausen Medical 2014". WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436. licensed CC BY 3.0 via Wikimedia Commons
- Exocrine and Endocrine Pancreas by OpenStax College, CC BY 3.0, via Wikimedia Commons
- Jaundice eye by CDC, public domain via Wikimedia Commons
- Symptoms of diabetes; licensed CC-0 via Wikimedia Commons
- Text adapted from Human Biology by CK-12 licensed CC BY-NC 3.0


