19.5: Thyroid Gland
- Page ID
- 92668
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\( \newcommand{\dsum}{\displaystyle\sum\limits} \)
\( \newcommand{\dint}{\displaystyle\int\limits} \)
\( \newcommand{\dlim}{\displaystyle\lim\limits} \)
\( \newcommand{\id}{\mathrm{id}}\) \( \newcommand{\Span}{\mathrm{span}}\)
( \newcommand{\kernel}{\mathrm{null}\,}\) \( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\) \( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\) \( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\id}{\mathrm{id}}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\kernel}{\mathrm{null}\,}\)
\( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\)
\( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\)
\( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\) \( \newcommand{\AA}{\unicode[.8,0]{x212B}}\)
\( \newcommand{\vectorA}[1]{\vec{#1}} % arrow\)
\( \newcommand{\vectorAt}[1]{\vec{\text{#1}}} % arrow\)
\( \newcommand{\vectorB}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vectorC}[1]{\textbf{#1}} \)
\( \newcommand{\vectorD}[1]{\overrightarrow{#1}} \)
\( \newcommand{\vectorDt}[1]{\overrightarrow{\text{#1}}} \)
\( \newcommand{\vectE}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash{\mathbf {#1}}}} \)
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\(\newcommand{\longvect}{\overrightarrow}\)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\(\newcommand{\avec}{\mathbf a}\) \(\newcommand{\bvec}{\mathbf b}\) \(\newcommand{\cvec}{\mathbf c}\) \(\newcommand{\dvec}{\mathbf d}\) \(\newcommand{\dtil}{\widetilde{\mathbf d}}\) \(\newcommand{\evec}{\mathbf e}\) \(\newcommand{\fvec}{\mathbf f}\) \(\newcommand{\nvec}{\mathbf n}\) \(\newcommand{\pvec}{\mathbf p}\) \(\newcommand{\qvec}{\mathbf q}\) \(\newcommand{\svec}{\mathbf s}\) \(\newcommand{\tvec}{\mathbf t}\) \(\newcommand{\uvec}{\mathbf u}\) \(\newcommand{\vvec}{\mathbf v}\) \(\newcommand{\wvec}{\mathbf w}\) \(\newcommand{\xvec}{\mathbf x}\) \(\newcommand{\yvec}{\mathbf y}\) \(\newcommand{\zvec}{\mathbf z}\) \(\newcommand{\rvec}{\mathbf r}\) \(\newcommand{\mvec}{\mathbf m}\) \(\newcommand{\zerovec}{\mathbf 0}\) \(\newcommand{\onevec}{\mathbf 1}\) \(\newcommand{\real}{\mathbb R}\) \(\newcommand{\twovec}[2]{\left[\begin{array}{r}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\ctwovec}[2]{\left[\begin{array}{c}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\threevec}[3]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\cthreevec}[3]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\fourvec}[4]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\cfourvec}[4]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\fivevec}[5]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\cfivevec}[5]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\mattwo}[4]{\left[\begin{array}{rr}#1 \amp #2 \\ #3 \amp #4 \\ \end{array}\right]}\) \(\newcommand{\laspan}[1]{\text{Span}\{#1\}}\) \(\newcommand{\bcal}{\cal B}\) \(\newcommand{\ccal}{\cal C}\) \(\newcommand{\scal}{\cal S}\) \(\newcommand{\wcal}{\cal W}\) \(\newcommand{\ecal}{\cal E}\) \(\newcommand{\coords}[2]{\left\{#1\right\}_{#2}}\) \(\newcommand{\gray}[1]{\color{gray}{#1}}\) \(\newcommand{\lgray}[1]{\color{lightgray}{#1}}\) \(\newcommand{\rank}{\operatorname{rank}}\) \(\newcommand{\row}{\text{Row}}\) \(\newcommand{\col}{\text{Col}}\) \(\renewcommand{\row}{\text{Row}}\) \(\newcommand{\nul}{\text{Nul}}\) \(\newcommand{\var}{\text{Var}}\) \(\newcommand{\corr}{\text{corr}}\) \(\newcommand{\len}[1]{\left|#1\right|}\) \(\newcommand{\bbar}{\overline{\bvec}}\) \(\newcommand{\bhat}{\widehat{\bvec}}\) \(\newcommand{\bperp}{\bvec^\perp}\) \(\newcommand{\xhat}{\widehat{\xvec}}\) \(\newcommand{\vhat}{\widehat{\vvec}}\) \(\newcommand{\uhat}{\widehat{\uvec}}\) \(\newcommand{\what}{\widehat{\wvec}}\) \(\newcommand{\Sighat}{\widehat{\Sigma}}\) \(\newcommand{\lt}{<}\) \(\newcommand{\gt}{>}\) \(\newcommand{\amp}{&}\) \(\definecolor{fillinmathshade}{gray}{0.9}\)The individual in Figure \(\PageIndex{1}\) has a goiter. A goiter is an abnormal enlargement of the thyroid gland, which is located in the neck. The formation of a goiter may occur in a number of different thyroid disorders. You’ll learn why in this concept.

Thyroid Structure
The thyroid gland is one of the largest endocrine glands in the body. It is located in the front of the neck below Adam’s apple (see Figure \(\PageIndex{2}\)). The gland is butterfly-shaped and composed of two lobes. The lobes are connected by a narrow band of thyroid tissue called an isthmus.
Internally, the thyroid gland is composed mainly of follicles. A follicle is a small cluster of cells surrounding a central cavity, which stores hormones and other molecules made by the follicular cells. Thyroid follicular cells are unique in being highly specialized to absorb and use iodine. They absorb iodine as iodide ions (I-) from the blood and use the iodide to produce thyroid hormones. The cells also use some of the iodide they absorb to form a protein called thyroglobulin, which serves to store iodide for later hormone synthesis. The outer layer of cells of each follicle secretes thyroid hormones as needed. Scattered among the follicles are another type of thyroid cells, called parafollicular cells (or C cells). These cells synthesize and secrete the hormone calcitonin.
Functions of the Thyroid
Like all endocrine glands, the function of the thyroid is to synthesize hormones and secrete them into the bloodstream. Once in the blood, they can travel to cells throughout the body and influence their functions.
Thyroid Hormones: T4 and T3
There are two main thyroid hormones produced by the follicles: thyroxine (T4), which contains four iodide ions and is represented by the structural diagram below; and triiodothyronine (T3), which contains three iodide ions. T3 is much more powerful than T4, but T4 makes up about 90 percent of circulating thyroid hormone, and T3 makes up only about 10 percent. However, most of the T4 is converted to T3 by target tissues.
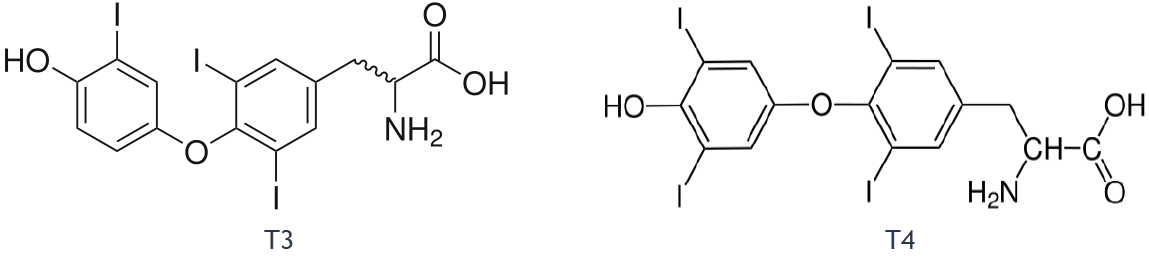
Figure \(\PageIndex{3}\): This structural model represents a single molecule of triiodothyronine (T3) and thyroxine (T4). The letter I represents the iodide ions they contain. The rings consist mainly of carbon atoms

Like steroid hormones, T3 and T4 cross cell membranes everywhere in the body and bind to intracellular receptors to regulate gene expression. However, unlike steroid hormones, thyroid hormones can cross cell membranes only with the help of special transporter proteins. Once inside the nucleus of cells, T3 and T4 turn on genes that control protein synthesis. Thyroid hormones increase the rate of metabolism in cells, so cells absorb more carbohydrates, use more energy, and produce more heat. Thyroid hormones also increase the rate and force of the heartbeat. In addition, they increase the sensitivity of cells to fight-or-flight hormones (that is, catecholamine hormones such as adrenaline).
The production of both T4 and T3 is regulated primarily by thyroid stimulating hormone (TSH), which is secreted by the anterior pituitary gland (see the diagram below). TSH production, in turn, is regulated by thyrotropin releasing hormone (TRH), which is produced by the hypothalamus. The thyroid gland, pituitary gland, and hypothalamus form a negative feedback loop to keep thyroid hormone secretion within a normal range. TRH and TSH production is suppressed when T4 levels start to become too high. The opposite occurs when T4 levels start to become too low.
Calcitonin
The calcitonin produced by the parafollicular cells of the thyroid gland has the role of helping to regulate blood calcium levels by stimulating the movement of calcium into bone. Calcitonin is secreted in response to rising blood calcium levels. It decreases blood calcium levels by enhancing calcium absorption and deposition in bone. Calcitonin works hand-in-hand with parathyroid hormone, which is secreted by the parathyroid glands and has the opposite effects as calcitonin. Together, these two hormones maintain calcium homeostasis.
Thyroid Disorders
As with other endocrine disorders, thyroid disorders are generally associated with either over or under-secretion of hormones. Abnormal secretion of thyroid hormones may occur for a variety of reasons.
Hyperthyroidism
Hyperthyroidism occurs when the thyroid gland produces excessive amounts of thyroid hormones. The most common cause of hyperthyroidism is Graves’ disease. Graves’ disease is an autoimmune disorder in which abnormal antibodies produced by the immune system stimulate the thyroid to secrete excessive quantities of its hormones. This stimulation overrides the usual negative feedback mechanism that normally controls thyroid hormone output. Graves’ disease often results in the formation of an enlarged thyroid (goiter) because of the continued stimulation to produce more hormones.
Besides a goiter, other signs and symptoms of hyperthyroidism may include protruding eyes (see photo below), heart palpitations, excessive sweating, diarrhea, weight loss despite increased appetite, muscle weakness, and unusual sensitivity to heat. Medications can be prescribed to mitigate the symptoms of the disease. Anti-thyroid drugs can also be given to decrease the production of thyroid hormones. If the drugs are ineffective, the gland can be partially or entirely removed. This can be done surgically or with the administration of radioactive iodine. Removal of the thyroid produces hypothyroidism.

Hypothyroidism
Hypothyroidism occurs when the thyroid gland produces insufficient amounts of thyroid hormones. It can result from surgical removal of the thyroid. However, worldwide, the most common cause of hypothyroidism is dietary iodine deficiency. In cases of iodine deficiency, the negative feedback loop controlling the release of thyroid hormone causes repeated stimulation of the thyroid. This results in the thyroid gland growing in size and producing a goiter. Although the gland gets larger, it cannot increase hormone output because of the lack of iodine in the diet.
Iodine deficiency is uncommon in the Western world because iodine is added to salt. Where iodine deficiency is not a problem, the most common cause of hypothyroidism is Hashimoto’s thyroiditis. This is another autoimmune disease, but in this case, the immune system destroys the thyroid gland, producing hypothyroidism. Hashimoto’s thyroiditis tends to run in families so it is likely to have a genetic component. It usually appears after the age of 30 and is more common in females than males.
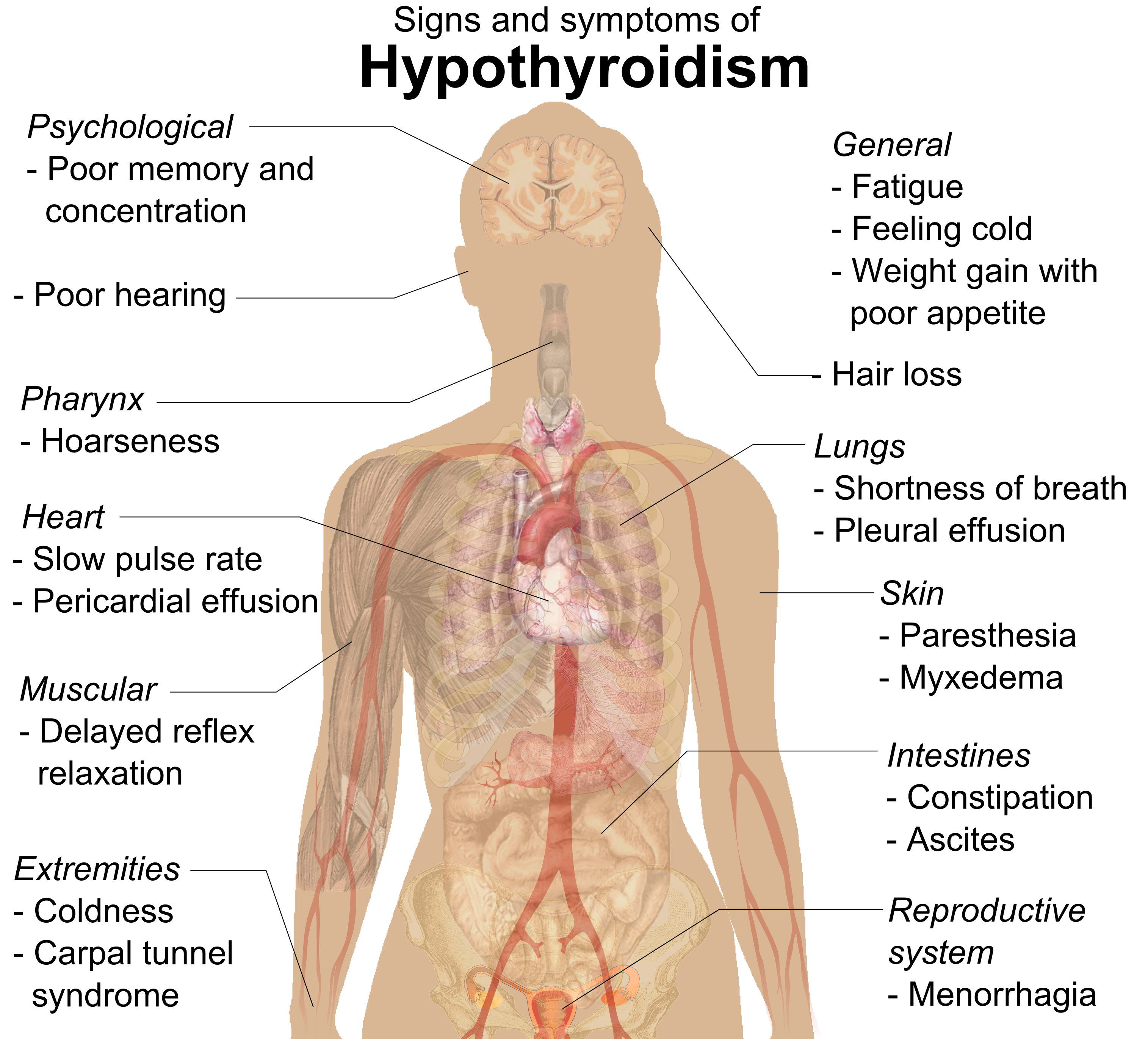
Hypothyroidism produces many signs and symptoms, as shown in Figure \(\PageIndex{6}\). These may include abnormal weight gain, tiredness, baldness, cold intolerance, and slow heart rate. Hypothyroidism is generally treated with thyroid hormone replacement therapy. This may be needed for the rest of a person’s life. Hypothyroidism in a pregnant woman can have serious adverse consequences for the fetus. During the fetal period, cells of the developing brain are a major target for thyroid hormones, which play a crucial role in brain maturation. When levels of thyroid hormones are too low, the fetus may suffer permanent deficits in cognitive abilities. Deafness is also a potential outcome of hypothyroidism in utero.
Feature: Myth vs. Reality
Thyroid disorders are relatively common, affecting as many as 20 million people in the United States. Because the disorders are common, there are also many common myths about them.
Myth: If you have a thyroid problem, you will know something is wrong because you will have obvious symptoms.
Reality: The majority of people with a thyroid disorder are not aware they have it because the symptoms are often mild, nonspecific, and easy to ignore. Generally, blood tests of thyroid hormone levels are needed to make a conclusive diagnosis.
Myth: If you are diagnosed with a thyroid disorder, you will have to take medication for the rest of your life.
Reality: Whether you need to continue thyroid medication for life depends on the cause of the disorder. For example, some women develop hypothyroidism during pregnancy but no longer need medication after the pregnancy is over and hormone levels return to normal.
Myth: As soon as you start taking thyroid medication, your symptoms will resolve.
Reality: It often takes weeks or even months for thyroid hormone levels to return to normal and symptoms to disappear.
Myth: You can take an over-the-counter iodine supplement to correct hypothyroidism.
Reality: In the United States, where dietary iodine is almost always adequate, iodine deficiency is unlikely to be the cause of hypothyroidism. Therefore, taking supplemental iodine is not likely to correct the problem.
Myth: If thyroid symptoms are mild, you don’t need to take medication.
Reality: Because thyroid hormones are responsible for so many vital body functions, failing to treat even a mild thyroid disorder may lead to a range of other problems, such as osteoporosis or infertility.
Myth: Goiter may be caused by eating “goitrogenic” vegetables, such as broccoli, Brussels sprouts, and spinach.
Reality: Although these foods can interfere with the thyroid’s ability to process iodide, you would have to eat huge amounts of them to cause goiter.
Myth: Thyroid disorders occur only after middle age and only in women.
Reality: Thyroid disorders may occur at any age and in any sex. Hypothyroidism occurs more commonly in older adults, but hyperthyroidism occurs more commonly in younger adults. Although women are more likely to develop thyroid disorders, about 20 percent of cases occur in men.
Review
- Describe the structure and location of the thyroid gland.
- Identify the types of cells within the thyroid gland that produce hormones.
- Compare and contrast T4 and T3.
- How do T4 and T3 affect body cells?
- Explain how T4 and T3 production is regulated.
- What is the function of calcitonin?
- Identify the chief cause and effects of hyperthyroidism.
- What are two possible causes of hypothyroidism?
- List signs and symptoms of hypothyroidism.
- Why may both hyperthyroidism and hypothyroidism cause goiters?
- Choose one symptom each for hyperthyroidism and hypothyroidism and explain why they occur based on the functions of thyroid hormones.
- Which hormone is produced by the thyroid gland?
- T3
- Calcitonin
- Parathyroid hormone
- TSH
- A and B
- In cases of hypothyroidism due to Hashimoto’s thyroiditis or removal of the thyroid gland to treat hyperthyroidism, patients are often given medication to replace the missing thyroid hormone. Explain why the level of replacement thyroid hormone must be carefully monitored and adjusted if needed.
- True or False. T3 and T4 bind to receptors on the plasma membrane of target cells.
- Which disease causes too much thyroid hormone to be produced?
- Hashimoto’s thyroiditis
- Graves’ disease
- Goiter
- Iodine deficiency
Explore More
Attributions
- Goiter by Almazi, public domain via Wikimedia Commons
- Thyroid by NIH, public domain via Arnavaz at French Wikipedia
- Triiodothyronine by Ayacop Public Domain via Wikimedia Commons
- Thyroxin chemical_structure by Wesalius; Public Domain via Wikimedia Commons
- Thyroid system
- Proptosis and lid retraction from Graves' Disease by Jonathan Trobe, M.D. - University of Michigan Kellogg Eye Center (The Eyes Have It), CC BY 3.0 via Wikimedia Commons
- Signs and symptoms of hypothyroidism by Mikael Häggström public domain via Wikimedia Commons
- Text adapted from Human Biology by CK-12 licensed CC BY-NC 3.0


