18.5: Adaptive Immune System
- Page ID
- 92732
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\( \newcommand{\dsum}{\displaystyle\sum\limits} \)
\( \newcommand{\dint}{\displaystyle\int\limits} \)
\( \newcommand{\dlim}{\displaystyle\lim\limits} \)
\( \newcommand{\id}{\mathrm{id}}\) \( \newcommand{\Span}{\mathrm{span}}\)
( \newcommand{\kernel}{\mathrm{null}\,}\) \( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\) \( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\) \( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\id}{\mathrm{id}}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\kernel}{\mathrm{null}\,}\)
\( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\)
\( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\)
\( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\) \( \newcommand{\AA}{\unicode[.8,0]{x212B}}\)
\( \newcommand{\vectorA}[1]{\vec{#1}} % arrow\)
\( \newcommand{\vectorAt}[1]{\vec{\text{#1}}} % arrow\)
\( \newcommand{\vectorB}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vectorC}[1]{\textbf{#1}} \)
\( \newcommand{\vectorD}[1]{\overrightarrow{#1}} \)
\( \newcommand{\vectorDt}[1]{\overrightarrow{\text{#1}}} \)
\( \newcommand{\vectE}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash{\mathbf {#1}}}} \)
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\(\newcommand{\longvect}{\overrightarrow}\)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
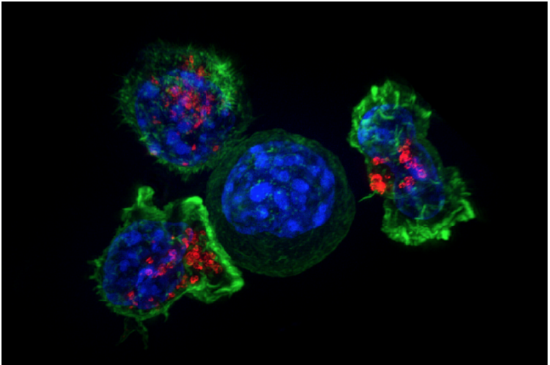
\(\newcommand{\avec}{\mathbf a}\) \(\newcommand{\bvec}{\mathbf b}\) \(\newcommand{\cvec}{\mathbf c}\) \(\newcommand{\dvec}{\mathbf d}\) \(\newcommand{\dtil}{\widetilde{\mathbf d}}\) \(\newcommand{\evec}{\mathbf e}\) \(\newcommand{\fvec}{\mathbf f}\) \(\newcommand{\nvec}{\mathbf n}\) \(\newcommand{\pvec}{\mathbf p}\) \(\newcommand{\qvec}{\mathbf q}\) \(\newcommand{\svec}{\mathbf s}\) \(\newcommand{\tvec}{\mathbf t}\) \(\newcommand{\uvec}{\mathbf u}\) \(\newcommand{\vvec}{\mathbf v}\) \(\newcommand{\wvec}{\mathbf w}\) \(\newcommand{\xvec}{\mathbf x}\) \(\newcommand{\yvec}{\mathbf y}\) \(\newcommand{\zvec}{\mathbf z}\) \(\newcommand{\rvec}{\mathbf r}\) \(\newcommand{\mvec}{\mathbf m}\) \(\newcommand{\zerovec}{\mathbf 0}\) \(\newcommand{\onevec}{\mathbf 1}\) \(\newcommand{\real}{\mathbb R}\) \(\newcommand{\twovec}[2]{\left[\begin{array}{r}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\ctwovec}[2]{\left[\begin{array}{c}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\threevec}[3]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\cthreevec}[3]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\fourvec}[4]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\cfourvec}[4]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\fivevec}[5]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\cfivevec}[5]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\mattwo}[4]{\left[\begin{array}{rr}#1 \amp #2 \\ #3 \amp #4 \\ \end{array}\right]}\) \(\newcommand{\laspan}[1]{\text{Span}\{#1\}}\) \(\newcommand{\bcal}{\cal B}\) \(\newcommand{\ccal}{\cal C}\) \(\newcommand{\scal}{\cal S}\) \(\newcommand{\wcal}{\cal W}\) \(\newcommand{\ecal}{\cal E}\) \(\newcommand{\coords}[2]{\left\{#1\right\}_{#2}}\) \(\newcommand{\gray}[1]{\color{gray}{#1}}\) \(\newcommand{\lgray}[1]{\color{lightgray}{#1}}\) \(\newcommand{\rank}{\operatorname{rank}}\) \(\newcommand{\row}{\text{Row}}\) \(\newcommand{\col}{\text{Col}}\) \(\renewcommand{\row}{\text{Row}}\) \(\newcommand{\nul}{\text{Nul}}\) \(\newcommand{\var}{\text{Var}}\) \(\newcommand{\corr}{\text{corr}}\) \(\newcommand{\len}[1]{\left|#1\right|}\) \(\newcommand{\bbar}{\overline{\bvec}}\) \(\newcommand{\bhat}{\widehat{\bvec}}\) \(\newcommand{\bperp}{\bvec^\perp}\) \(\newcommand{\xhat}{\widehat{\xvec}}\) \(\newcommand{\vhat}{\widehat{\vvec}}\) \(\newcommand{\uhat}{\widehat{\uvec}}\) \(\newcommand{\what}{\widehat{\wvec}}\) \(\newcommand{\Sighat}{\widehat{\Sigma}}\) \(\newcommand{\lt}{<}\) \(\newcommand{\gt}{>}\) \(\newcommand{\amp}{&}\) \(\definecolor{fillinmathshade}{gray}{0.9}\)The photomicrograph in Figure \(\PageIndex{1}\) shows a group of killer T cells (green and red) surrounding a cancer cell (blue, center). When a killer T cell makes contact with the cancer cell, it attaches to and spreads over the dangerous target. The killer T cell then uses special chemicals stored in vesicles (red) to deliver the killing blow. This event has thus been nicknamed “the kiss of death.” After the target cell is killed, the killer T cells move on to find the next victim. Killer T cells like these are important players in the adaptive immune system.
The adaptive immune system is a subsystem of the overall immune system. It is composed of highly specialized cells and processes that eliminate specific pathogens and tumor cells. An adaptive immune response is set in motion by antigens that the immune system recognizes as foreign. Unlike an innate immune response, an adaptive immune response is highly specific to a particular pathogen (or its antigen). An important function of the adaptive immune system that is not shared by the innate immune system is the creation of immunological memory or immunity. This occurs after the initial response to a specific pathogen. It allows a faster, stronger response on subsequent encounters with the same pathogen, usually before the pathogen can cause symptoms of illness.
Lymphocytes are the main cells of the adaptive immune system. They are leukocytes that arise and mature in organs of the lymphatic system, including the bone marrow and thymus. The human body normally has about 2 trillion lymphocytes, which constitute about a third of all leukocytes. Most of the lymphocytes are normally sequestered within tissue fluid or organs of the lymphatic system, including the tonsils, spleen, and lymph nodes. Only about 2 percent of the lymphocytes are normally circulating in the blood. There are two main types of lymphocytes involved in adaptive immune responses, called T cells and B cells. T cells destroy infected cells or release chemicals that regulate immune responses. B cells secrete antibodies that bind with antigens of pathogens so they can be removed by other immune cells or processes.
T Cells
There are multiple types of T cells or T lymphocytes. Major types are killer (or cytotoxic) T cells and helper T cells. Both types develop from immature T cells that become activated by exposure to an antigen.
T Cell Activation
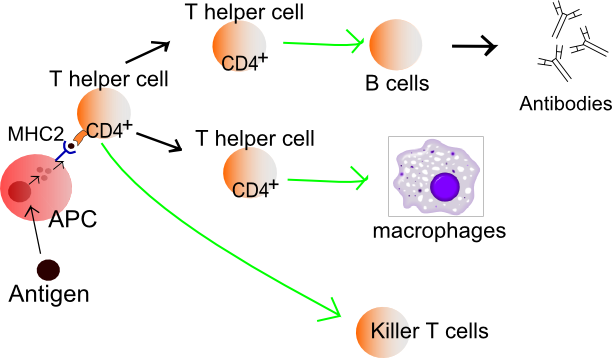
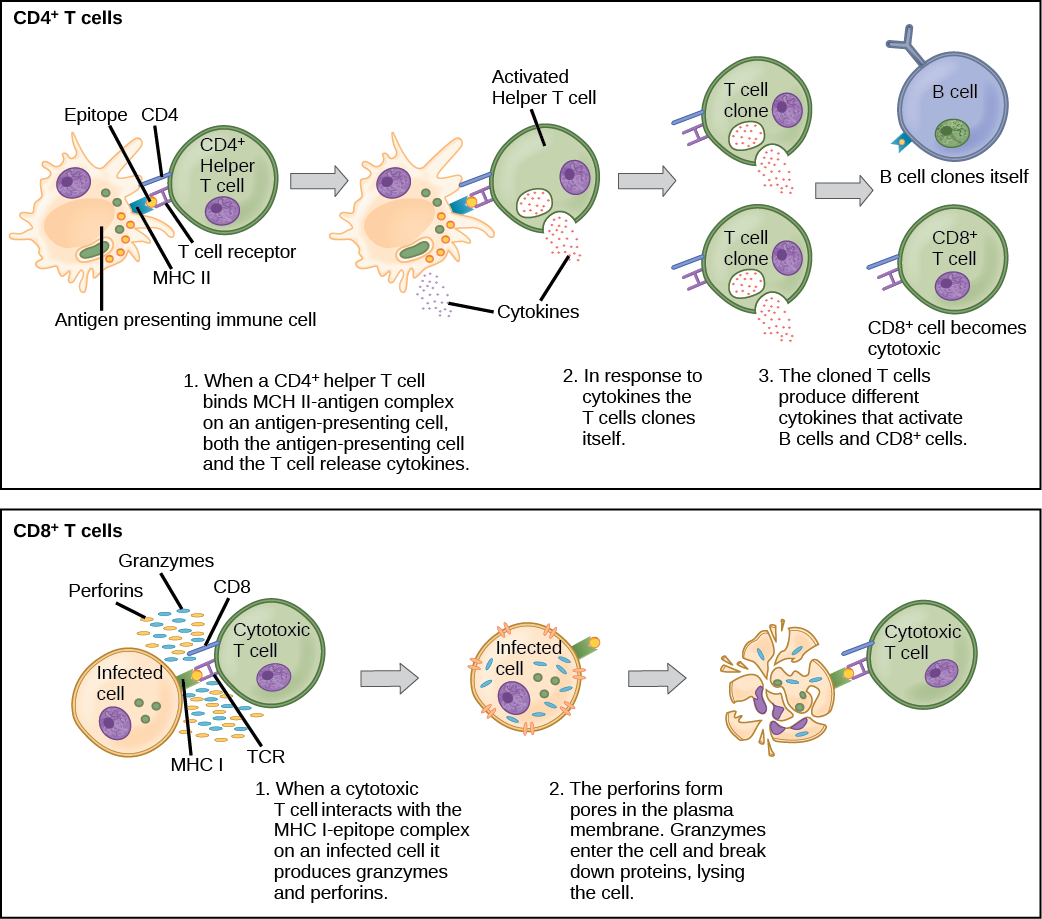
T cells must be activated. After the pathogen is phagocytized and digested by macrophages, a part of the pathogen is displayed on the surface of the macrophage. The proteins that display the antigen (part of the pathogen) are called Major Histocompatibility Complex (MHC). There are two types of MHC, MHCI and MHCII. Therefore macrophages are called antigen-presenting cells as shown in Figure \(\PageIndex{2}\) and Figure \(\PageIndex{3}\). B lymphocytes can also act as antigen-presenting cells. Helper T cells are more easily activated than killer T cells. Activation of killer T cells is strongly regulated and may require additional stimulation from helper T cells.
Helper T Cells
Activated helper T cells do not kill infected or cancerous cells. Instead, their role is to “manage” both innate and adaptive immune responses by directing other cells to perform these tasks. They control other cells by releasing cytokines. These are proteins that can influence the activity of many cell types, including cytotoxic killer T cells (sometimes referred to as only killer T cells), B cells, and macrophages. For example, some cytokines released by helper T cells help activate killer T cells.
Killer T Cells (Cytotoxic T Cells)
When infected body cells present pathogen antigen to a killer T cell, it gets activated (see lower panel of Figure \(\PageIndex{3}\)). Activated killer T cells induce the death of cells that bear a specific non-self antigen because they are infected with pathogens or are cancerous. The antigen targets the cell for destruction by killer T cells, which travel through the bloodstream searching for target cells to kill. Killer T cells may use various mechanisms to kill target cells. One way is by releasing toxins in granules that enter and kill infected or cancerous cells (Figure \(\PageIndex{3}\)).
B Cells and B Cell Activation
B cells, or B lymphocytes, are the major cells involved in the creation of antibodies that circulate in blood plasma and lymph. Antibodies are large, Y-shaped proteins used by the immune system to identify and neutralize foreign invaders. Besides producing antibodies, B cells may also function as antigen-presenting cells or secrete cytokines that help control other immune cells and responses.
Before B cells can actively function to defend the host, they must be activated. As shown in Figure \(\PageIndex{4}\), B cell activation begins when a B cell engulfs and digests an antigen. The antigen may be either free-floating or on top of the pathogen. B cell internalize antigen and present it on its MHC to a helper T cell. The T cell activates and secretes cytokines that help the B cell to multiply and the daughter cells to mature into plasma cells and memory B cells. Plasma B cells produce antibodies.
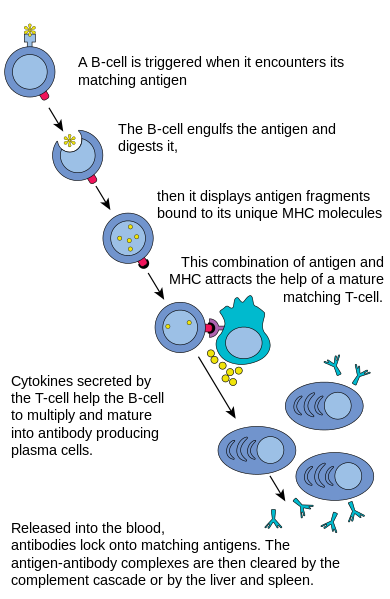
Plasma Cells
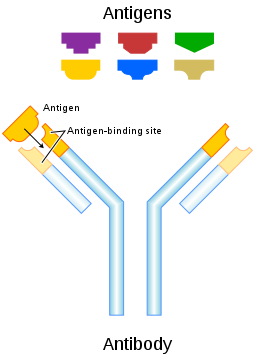
Plasma cells are antibody-secreting cells that form from activated B cells. Each plasma cell is like a tiny antibody factory. It may secrete millions of copies of an antibody, each of which can bind to the specific antigen that activated the original B cell. The specificity of an antibody to a specific antigen is illustrated in Figure \(\PageIndex{5}\). When antibodies bind with antigens, it makes the cells bearing them easier targets for phagocytes to find and destroy. Antibody-antigen complexes may also trigger the complement system of the innate immune system, which destroys the cells in a cascade of protein enzymes. In addition, the complexes are likely to clump together (agglutinate). If this occurs, they are filtered out of the blood in the spleen or liver.
Immunity
Most activated T cells and B cells die within a few days once a pathogen has been cleared from the body. However, a few of the cells survive and remain in the body as memory T cells or memory B cells. These memory cells are ready to activate an immediate response if they are exposed to the same antigen again in the future. This is the basis of immunity.
The earliest known reference to the concept of immunity relates to the bubonic plague (see Figure \(\PageIndex{6}\)). In 430 B.C., a Greek historian and general named Thucydides noted that people who had recovered from a previous bout of the plague could nurse people sick with the plague without contracting the illness a second time. We now know that this is true of many diseases and it occurs because of active immunity.

Active Immunity
Active immunity is the ability of the adaptive immune system to resist a specific pathogen because it has formed an immunological memory of the pathogen. Active immunity is adaptive because it occurs during the lifetime of an individual as an adaptation to infection with a specific pathogen and prepares the immune system for future challenges from that pathogen. Active immunity can come about naturally or artificially.
Naturally Acquired Active Immunity
Active immunity is acquired naturally when a pathogen invades the body and activates the adaptive immune system. When the initial infection is over, memory B cells and memory T cells remain that provide immunological memory of the pathogen. As long as the memory cells are alive, the immune system is ready to mount an immediate response if the same pathogen tries to infect the body again.
Artificially Acquired Active Immunity
Active immunity can also be acquired artificially through immunization. Immunization is the deliberate exposure of a person to a pathogen in order to provoke an adaptive immune response and the formation of memory cells specific to that pathogen. The pathogen is introduced in a vaccine — usually by injection, sometimes by nose or mouth (Figure \(\PageIndex{7}\)) — so immunization is also called vaccination.
In a vaccine, only part of a pathogen, a weakened form of the pathogen, or a dead pathogen is typically used. This causes an adaptive immune response without making the immunized person sick. This is how you most likely became immune to diseases such as measles, mumps, and chickenpox. Immunizations may last for a lifetime or require periodic booster shots to maintain immunity. While immunization generally has long-lasting effects, it usually takes several weeks to develop full immunity.
Immunization is the most effective method ever discovered in preventing infectious diseases. As many as 3 million deaths are prevented each year because of vaccinations. Widespread immunity due to vaccinations is largely responsible for the worldwide eradication of smallpox and the near elimination of several other infectious diseases from many populations, including such diseases as polio and measles. Immunization is so successful because it exploits the natural specificity and inducibility of the adaptive immune system.
Passive Immunity
Passive immunity results when pathogen-specific antibodies or activated T cells are transferred to a person who has never been exposed to the pathogen. Passive immunity provides immediate protection from a pathogen, but the adaptive immune system does not develop immunological memory to protect the host from the same pathogen in the future. Unlike active immunity, passive immunity lasts only as long as the transferred antibodies or T cells survive in the blood. This is usually between a few days and a few months. However, like active immunity, passive immunity can be acquired both naturally and artificially.
Naturally Acquired Passive Immunity
Passive immunity is acquired naturally by a fetus through its mother’s blood. Antibodies are transported from mother to fetus across the placenta, so babies have high levels of antibodies at birth. Their antibodies have the same range of antigen specificity as their mother’s. Passive immunity may also be acquired by an infant through the mother’s breast milk. This gives young infants protection from common pathogens in their environment while their own immune system matures.
Artificially Acquired Passive Immunity
Older children and adults can acquire passive immunity artificially through the injection of antibodies or activated T cells. This may be done when there is a high risk of infection and insufficient time for the body to develop active immunity through vaccination. It may also be done to reduce symptoms of ongoing disease or to compensate for immunodeficiency diseases (for the latter, see the concept Disorders of the Immune System).
Adaptive Immune Evasion
Many pathogens have been around for a long time, living with human populations for generations. To persist, some have evolved mechanisms to evade the adaptive immune system of human hosts. One way they have done this is by rapidly changing their non-essential antigens. This is called antigenic variation. An example of a pathogen that takes this approach is the human immunodeficiency virus (HIV). It mutates rapidly so the proteins on its viral envelope are constantly changing. By the time the adaptive immune system responds, the virus’s antigens have changed. Antigenic variation is the main reason that efforts to develop a vaccine against HIV have not yet been successful.
Another evasion approach some pathogens may take is to mask pathogen antigens with host molecules so the host’s immune system cannot detect the antigens. HIV takes this approach as well. The envelope that covers the virus is formed from the outermost membrane of the host cell.
If you think that immunizations are just for kids, think again. There are several vaccines recommended by the CDC for people over the age of 18. This link shows the vaccine schedule recommended for all adults aged 19 years and older. Additional vaccines may be recommended for certain adults based on specific medical conditions or other indications. Are you up to date with your vaccines? You can check with your doctor to be sure.
Review
- What is the adaptive immune system?
- Describe the main cells of the adaptive immune system.
- How are lymphocytes activated?
- Identify two common types of T cells and their functions.
- How do activated B cells help defend against pathogens?
- Define immunity.
- What are two ways active immunity may come about?
- How does passive immunity differ from active immunity?
- How may passive immunity occur?
- What ways of evading the human adaptive immune system evolved in the human immunodeficiency virus (HIV)?
- Describe two ways in which B cells and T cells work together to generate adaptive immune responses.
- Which cells directly kill pathogen-infected or cancerous cells?
- A. Plasma cells
- B. Killer T cells
- C. Helper T cells
- D. All of the above
- Why do vaccinations involve the exposure of a person to a version of a pathogen?
- True or False. Immunization is a form of passive immunity.
- True or False. Antibodies transmitted from mother to child via breast milk cause the formation of memory B cells and long-term immunity.
Explore More
Watch this video to learn about the recent status of HIV vaccine development:
Attributions
- Killer T cells surrounded by Cancer Cells by NIH, Public Domain via Wikimedia Commons
- T cell receptors by Charles Molnar, CC BY 4.0 via BC Campus
- Lymphocyte activation by Mikael Häggström, public domain via Wikimedia Commons
- B cell activation by Fred the Oyster, public domain via Wikimedia Commons
- Antibody by Fvasconcellos, Public domain via Wikimedia Commons
- Acral gangrene of digits by CDC, Public Domain via Wikimedia Commons
- Polio drops by USAID, Public Domain, via Wikimedia Commons
- Text adapted from Human Biology by CK-12 licensed CC BY-NC 3.0


