16.6: Glycoproteins and Human Health
- Page ID
- 89006
We’ll close this chapter with a few examples of glycoproteins that play crucial roles in human physiology. Let’s look first at the major human A, B, AB, O, and Rh blood groups that result from the presence or absence of glycoprotein antigens embedded in red blood cell membranes and the presence or absence in the blood of antibodies against the antigens. Typically, an exposure to antigens (e.g., foreign substances like bacteria, viruses, and toxins) generates immunoglobulins, the antibody molecules of our immune system. The immunoglobulins are glycoproteins. Since blood-group antibodies already in the blood of a healthy person are not a response to foreign antigen invasion, they are something of a paradox!
You probably know that blood groups must be compatible for a successful blood transfusion. A mismatch between donor and recipient can be devastating. An interaction of the red-cell antigens of one blood group with antibodies in another blood group will cause the red cells to clump, restricting blood flow, and ultimately killing the transfusion recipient. Figure 16.20 summarizes why transfusions with mismatched A, B, AB, and O blood groups must be avoided.
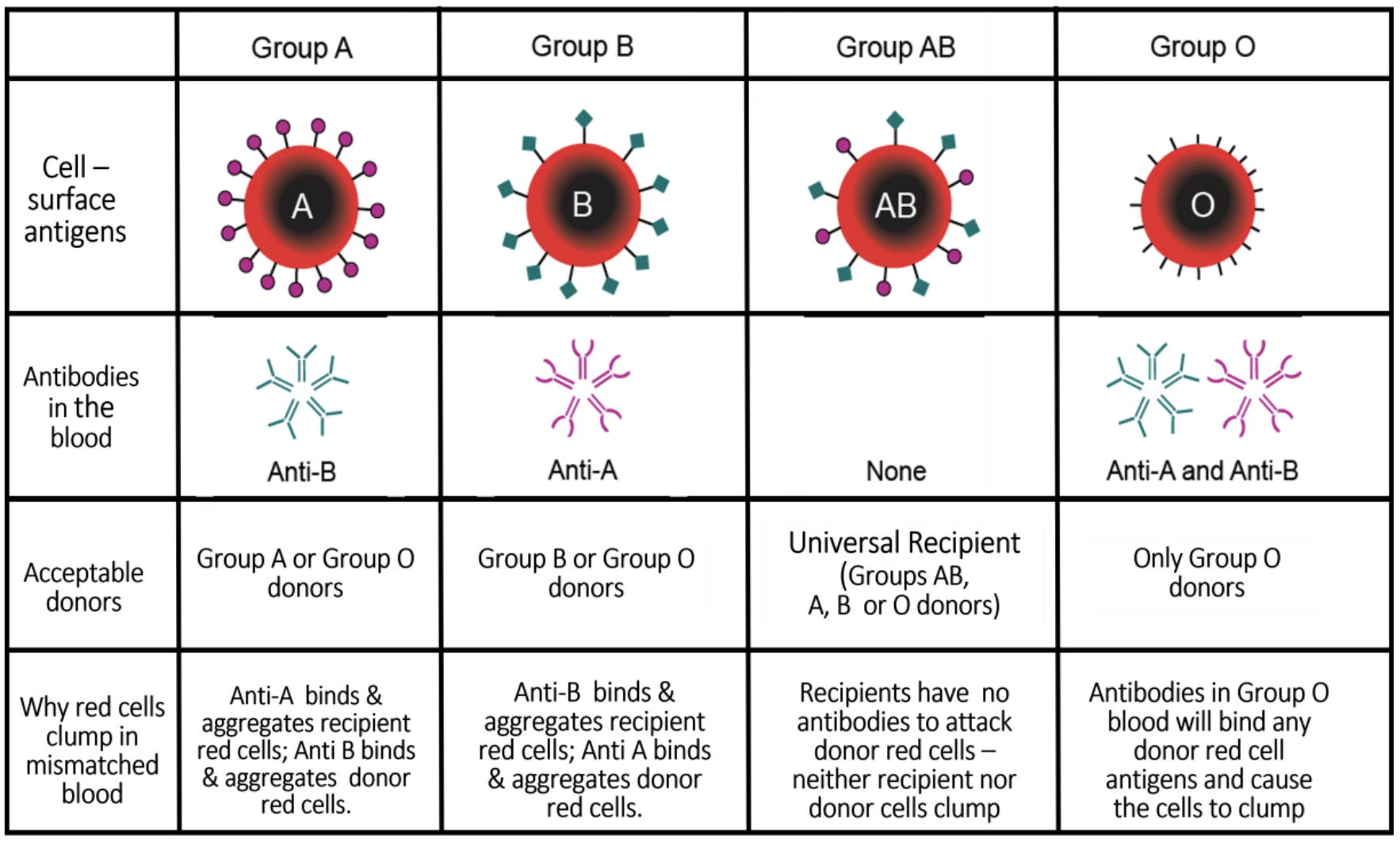
From the table above, you can see why type O blood is called the universal donor and is thus in high demand by clinics and hospitals.
Now, thanks to enzymes produced by members of the gut microbiome, the absolute requirement that blood groups must be matched for safe transfusions may someday be a thing of the past! One of these enzymes is a glycosidase that can digest the sugars on A and B antigens on the surfaces of A, B, and AB blood cells. This effectively converts them to type O red blood cells! Check the Red Cross website (About A, B, AB, & O Blood Types-Red Cross) or Wikipedia (Other Blood Types) for more details about blood groups. See Conversion of A, B & AB to O for a summary of recent research on enzymatically converting all blood types to type O.
Another red blood cell antigen is the Rh (rhesus) factor. Rhesus factors are antigens originally found to define blood types in rhesus monkeys, but humans have equivalent antigens, so human Rh blood groups have nothing to do with the monkeys! People either have their own Rh factor and are \(\rm Rh^{+}\), or they don’t have the factor and are \(\rm Rh^{−}\).
When an \(\rm Rh^{−}\) recipient is transfused with blood from an \(\rm Rh^{+}\) donor, the recipient’s immune system makes anti-Rh antibodies in the usual way. This too can cause blood-cell clumping with bad consequences. A well-known example is when an Rh− pregnant woman is carrying an \(\rm Rh^{+}\) fetus; if mother and baby’s blood should mix, the mother will make antibodies to the Rh factor that could cause fetal hemolytic disease, damaging and destroying fetal red blood cells.
A word to the wise: While you should be “typed” in the event you need a transfusion, it’s always a good idea to know your own ABO and Rh blood groups!
The basis of selection of the different blood groups is something of a mystery. What benefit did they confer on us at the time of selection, and do we still benefit today? Check out a discussion of blood group evolution at Evolution of Blood Groups, and briefly summarize any one part of the discussion that grabs your interest.
The last example here involves cell surface antigens of the MHC (Major Histocompatibility Complex) glycoproteins that distinguish self from nonself in body tissues and organs. Transplantation of liver, kidneys, heart, and other major organs, from donors into patients with failing organs has become if not routine, then at least increasingly common. Before a transplant, MHC tissue typing determines donor and recipient compatibility to reduce the chances of the rejection of the transplanted organ. Since available donors are few and good matches even fewer, patients wait on prioritized lists for a matched organ. Even when MHC typing is a match, the transplant recipient’s immune system must be suppressed with hormones to further reduce chances of rejection. Unlike the limited number of blood groups, there are many MHC proteins that must be analyzed to determine a match. Thus, it is not practical (or routinely necessary) to “know” your MHC type! In the next chapter, we look at membrane functions intrinsic to cellular existence itself.


