16.4: Disorders of the Respiratory System
- Page ID
- 16820
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\( \newcommand{\id}{\mathrm{id}}\) \( \newcommand{\Span}{\mathrm{span}}\)
( \newcommand{\kernel}{\mathrm{null}\,}\) \( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\) \( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\) \( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\id}{\mathrm{id}}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\kernel}{\mathrm{null}\,}\)
\( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\)
\( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\)
\( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\) \( \newcommand{\AA}{\unicode[.8,0]{x212B}}\)
\( \newcommand{\vectorA}[1]{\vec{#1}} % arrow\)
\( \newcommand{\vectorAt}[1]{\vec{\text{#1}}} % arrow\)
\( \newcommand{\vectorB}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vectorC}[1]{\textbf{#1}} \)
\( \newcommand{\vectorD}[1]{\overrightarrow{#1}} \)
\( \newcommand{\vectorDt}[1]{\overrightarrow{\text{#1}}} \)
\( \newcommand{\vectE}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash{\mathbf {#1}}}} \)
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\(\newcommand{\avec}{\mathbf a}\) \(\newcommand{\bvec}{\mathbf b}\) \(\newcommand{\cvec}{\mathbf c}\) \(\newcommand{\dvec}{\mathbf d}\) \(\newcommand{\dtil}{\widetilde{\mathbf d}}\) \(\newcommand{\evec}{\mathbf e}\) \(\newcommand{\fvec}{\mathbf f}\) \(\newcommand{\nvec}{\mathbf n}\) \(\newcommand{\pvec}{\mathbf p}\) \(\newcommand{\qvec}{\mathbf q}\) \(\newcommand{\svec}{\mathbf s}\) \(\newcommand{\tvec}{\mathbf t}\) \(\newcommand{\uvec}{\mathbf u}\) \(\newcommand{\vvec}{\mathbf v}\) \(\newcommand{\wvec}{\mathbf w}\) \(\newcommand{\xvec}{\mathbf x}\) \(\newcommand{\yvec}{\mathbf y}\) \(\newcommand{\zvec}{\mathbf z}\) \(\newcommand{\rvec}{\mathbf r}\) \(\newcommand{\mvec}{\mathbf m}\) \(\newcommand{\zerovec}{\mathbf 0}\) \(\newcommand{\onevec}{\mathbf 1}\) \(\newcommand{\real}{\mathbb R}\) \(\newcommand{\twovec}[2]{\left[\begin{array}{r}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\ctwovec}[2]{\left[\begin{array}{c}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\threevec}[3]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\cthreevec}[3]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\fourvec}[4]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\cfourvec}[4]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\fivevec}[5]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\cfivevec}[5]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\mattwo}[4]{\left[\begin{array}{rr}#1 \amp #2 \\ #3 \amp #4 \\ \end{array}\right]}\) \(\newcommand{\laspan}[1]{\text{Span}\{#1\}}\) \(\newcommand{\bcal}{\cal B}\) \(\newcommand{\ccal}{\cal C}\) \(\newcommand{\scal}{\cal S}\) \(\newcommand{\wcal}{\cal W}\) \(\newcommand{\ecal}{\cal E}\) \(\newcommand{\coords}[2]{\left\{#1\right\}_{#2}}\) \(\newcommand{\gray}[1]{\color{gray}{#1}}\) \(\newcommand{\lgray}[1]{\color{lightgray}{#1}}\) \(\newcommand{\rank}{\operatorname{rank}}\) \(\newcommand{\row}{\text{Row}}\) \(\newcommand{\col}{\text{Col}}\) \(\renewcommand{\row}{\text{Row}}\) \(\newcommand{\nul}{\text{Nul}}\) \(\newcommand{\var}{\text{Var}}\) \(\newcommand{\corr}{\text{corr}}\) \(\newcommand{\len}[1]{\left|#1\right|}\) \(\newcommand{\bbar}{\overline{\bvec}}\) \(\newcommand{\bhat}{\widehat{\bvec}}\) \(\newcommand{\bperp}{\bvec^\perp}\) \(\newcommand{\xhat}{\widehat{\xvec}}\) \(\newcommand{\vhat}{\widehat{\vvec}}\) \(\newcommand{\uhat}{\widehat{\uvec}}\) \(\newcommand{\what}{\widehat{\wvec}}\) \(\newcommand{\Sighat}{\widehat{\Sigma}}\) \(\newcommand{\lt}{<}\) \(\newcommand{\gt}{>}\) \(\newcommand{\amp}{&}\) \(\definecolor{fillinmathshade}{gray}{0.9}\)The scary beast in Figure \(\PageIndex{1}\) is likely to be lurking in your own home, where it feeds on organic debris, including human skin. What is it? It’s the common dust mite, a close relative of spiders. The dust mite is so small that it is barely visible with the unaided eye, so it’s obviously shown above greatly enlarged. If you think you can get rid of dust mites in your home by frequent and thorough cleaning, think again. There may be thousands of dust mites in just one gram of dust! Regardless of how clean you keep your house, you can't eliminate dust mites entirely. So why even bother trying? The feces of dust mites contain proteins that are a common trigger of asthma attacks.

Asthma
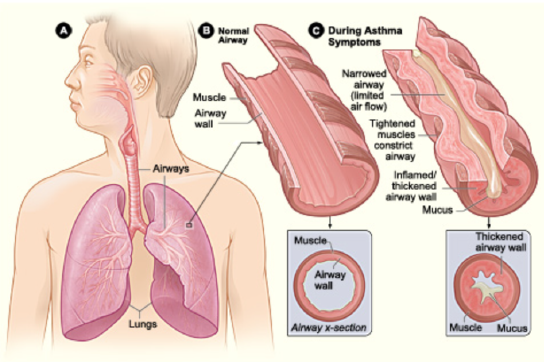
Asthma is a chronic inflammatory disease of the airways in the lungs, in which the airways periodically become inflamed. As you can see in Figure \(\PageIndex{2}\), this causes swelling and narrowing of the airways, often accompanied by excessive mucus production. Symptoms of asthma include difficulty breathing, coughing, wheezing, shortness of breath, and chest tightness. Some people with asthma rarely experience symptoms, and then usually only in response to certain triggers in the environment. Other people may have symptoms almost all of the time.
Asthma is thought to be caused by a combination of genetic and environmental factors. A person with a family history of asthma is more likely to develop the disease. Dozens of genes have been found to be associated with asthma, many of which are related to the immune system. Additional risk factors include obesity and sleep apnea (see the feature My Human Body below). Environmental factors trigger asthma attacks in people who have a genetic predisposition to the disease. Besides dust mite feces, triggers may include other allergens (such as pet dander, cockroaches, and mold), certain medications including aspirin, air pollution, and stress, among other possible factors. Symptoms tend to be worse at night and early in the morning. They may also worsen during upper respiratory tract infections, strenuous exercise, or when the airways are exposed to cold air.
There is no cure for asthma at present, but the symptoms of asthma attacks usually can be reversed with the use of inhaled medications called bronchodilators. These medications soothe the constricted air passages and help to re-expand them, making breathing easier. The medications usually start to take effect almost immediately. Other medications can be taken for long-term control of the disease. These medications help prevent asthma attacks from occurring. Corticosteroids are generally considered the most effective treatment for long-term control. Another way to prevent asthma attacks is by avoiding triggers whenever possible.
Pneumonia
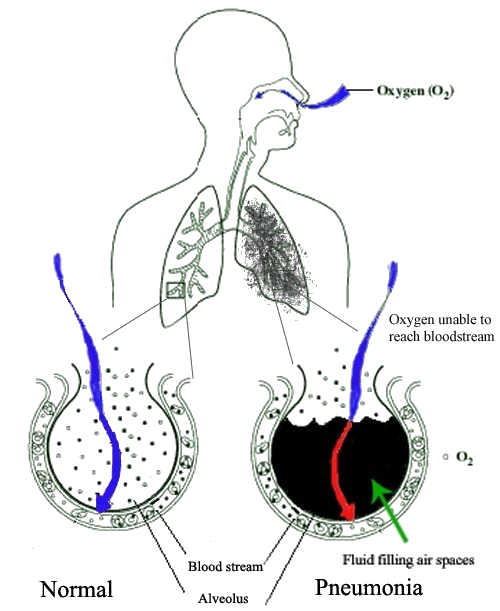
Another common inflammatory disease of the respiratory tract is pneumonia. In pneumonia, the inflammation affects primarily the alveoli, which are the tiny air sacs of the lungs. Inflammation causes some of the alveoli to become filled with fluid so that gas exchange cannot occur. This is illustrated in Figure \(\PageIndex{3}\). Symptoms of pneumonia typically include coughing, chest pain, difficulty breathing, and fever.
Pneumonia often develops as a consequence of an upper respiratory tract infection such as the common cold or flu, especially in the very young and the elderly. It is usually caused by bacteria or viruses, although some cases may be caused by other microorganisms such as fungi. The majority of cases are caused by just a few pathogens, the most common being the bacterium Streptococcus pneumoniae. Pneumonia is more likely to develop in people who have other lung diseases such as asthma, a history of smoking, heart failure, or a weakened immune system.
Vaccines are available to prevent certain types of bacterial and viral pneumonia, including pneumonia caused by Streptococcus pneumoniae. Treatment of pneumonia depends on the cause. For example, if it is caused by bacteria, antibiotics are generally prescribed. In cases of severe pneumonia, hospitalization and supplemental oxygen may be required.
Chronic Obstructive Pulmonary Disease
Chronic obstructive pulmonary disease (COPD) is a lung disease characterized by chronic poor airflow. The main symptoms include shortness of breath and a cough that produces phlegm. These symptoms are usually present for a long period of time and typically become worse over time. Eventually, walking upstairs and similar activities become difficult because of shortness of breath.
COPD formerly was referred to as chronic bronchitis or emphysema. Now, the term chronic bronchitis is used to refer to the symptoms of COPD, and the term emphysema is used to refer to the lung changes that occur with COPD. Some of these lung changes are shown in Figure \(\PageIndex{4}\). They include a breakdown of connective tissues that reduces the number and elasticity of alveoli. As a result, the patient can no longer fully exhale air from the lungs, so the air becomes trapped in the lungs. Gas exchange is hampered and may lead to low oxygen levels and too much carbon dioxide in the blood.
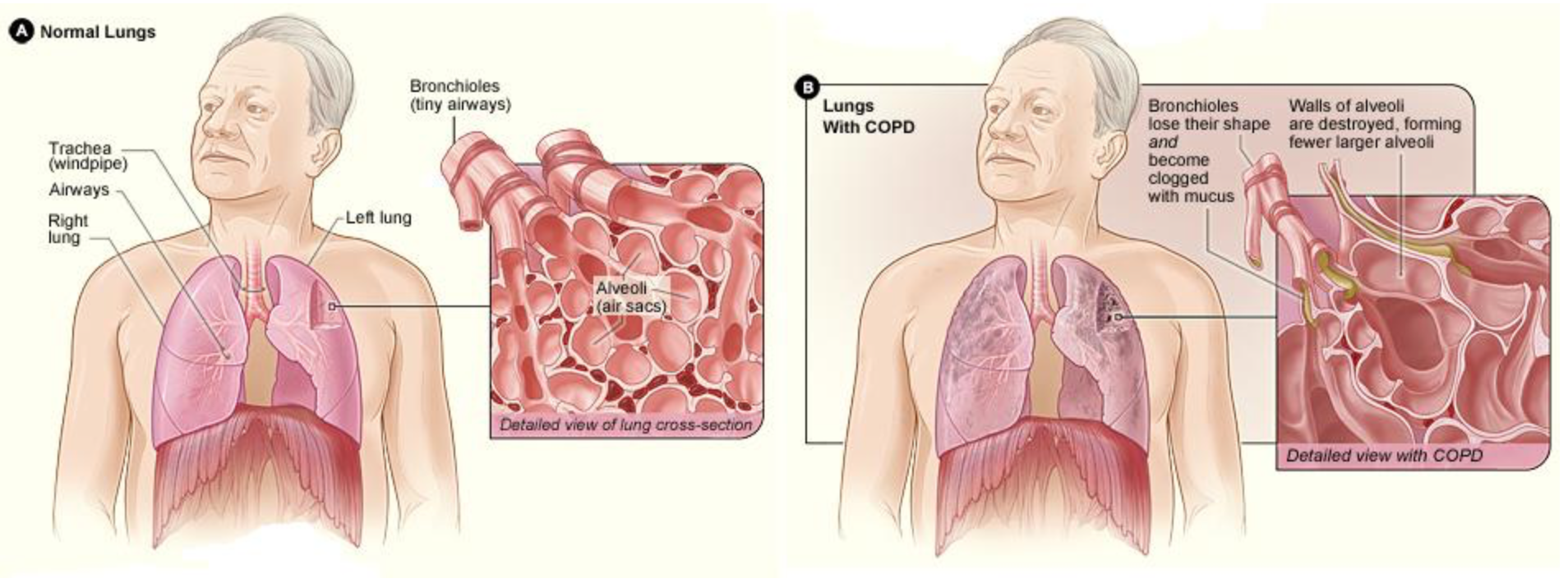
Tobacco smoking is the major cause of COPD, with a number of other factors such as air pollution and genetics playing smaller roles. Of people who are life-long smokers, about half will eventually develop COPD. Exposure to secondhand smoke in nonsmokers also increases the risk of COPD and accounts for about 20 percent of cases. Most cases of COPD could have been prevented by never smoking. In people who have already been diagnosed with COPD, cessation of smoking can slow down the rate at which COPD worsens. People with COPD may be treated with supplemental oxygen and inhaled bronchodilators. These treatments may reduce the symptoms but there is no cure for COPD except, in very severe cases, lung transplantation (see the Explore More video below).
Lung Cancer
Lung cancer is a malignant tumor characterized by uncontrolled cell growth in tissues of the lung. The tumor may arise directly from lung tissue (primary lung cancer) or as a result of metastasis from cancer in another part of the body (secondary lung cancer). Primary lung cancer may also metastasize and spread to other parts of the body. Lung cancer develops following genetic damage to DNA that affects the normal functions of the cell. As more damage accumulates, the risk of cancer increases. The most common symptoms of lung cancer include coughing (especially coughing up blood), wheezing, shortness of breath, chest pain, and weight loss.
The major cause of primary lung cancer is tobacco smoking, which accounts for about 85 percent of cases. Cigarette smoke contains numerous cancer-causing chemicals. Besides smoking, other potential causes of lung cancer include exposure to radon gas, asbestos, secondhand smoke, or other air pollutants. When tobacco smoking is combined with other risk factors such as exposure to radon or asbestos, the risk of lung cancer is heightened. People who have close biological relatives with lung cancer are also at increased risk of developing the disease.
Most cases of lung cancer cannot be cured. In many people, cancer has already spread beyond the original site by the time they have symptoms and seek medical attention. About 10 percent of people with lung cancer do not have symptoms when they are diagnosed, and the cancers are found when they have a chest X-ray for another problem. In part because of its typically late diagnosis, lung cancer is the most common cause of cancer-related death in men and the second most common cause in women (after breast cancer). Common treatments for lung cancer include surgical removal of the tumor, radiation therapy, chemotherapy, or some combination of these three types of treatment.
Do you — or someone you love — snore? Snoring may be more than just an annoyance. It may also be a sign of a potentially dangerous and common disorder known as sleep apnea. Sleep apnea is characterized by pauses in breathing that occur most often because of physical blockage to airflow during sleep. When breathing is paused, carbon dioxide builds up in the bloodstream. The higher-than-normal level of carbon dioxide in the blood causes the respiratory centers in the brain to wake the person enough to start breathing normally. This reduces the carbon dioxide level, and the person falls back asleep. This occurs repeatedly throughout the night, causing serious disruption in sleep. Most people with sleep apnea are unaware that they have the disorder because they don’t awake fully enough to remember the repeated awakenings throughout the night. Instead, sleep apnea is more commonly recognized by other people who witness the episodes.
Figure \(\PageIndex{5}\)shows how sleep apnea typically occurs. The muscle tone of the body normally relaxes during sleep, allowing the soft tissues in the throat to collapse and block the airway. The relaxation of muscles may be exacerbated by the use of alcohol, tranquilizers, or muscle relaxants. The risk of sleep apnea is greater in people who are overweight, smoke tobacco, or have diabetes. The disorder is also more likely to occur in older people and males. Common symptoms of sleep apnea include loud snoring, restless sleep, and daytime sleepiness and fatigue. Daytime sleepiness, in turn, increases the risk of driving and work-related accidents. Continued sleep deprivation may cause moodiness and belligerence. Lack of adequate oxygen to the body because of sleep apnea may also lead to other health problems including fatty liver diseases and high blood pressure. Symptoms of sleep apnea may be present for years or even decades until (and if) a diagnosis is finally made.
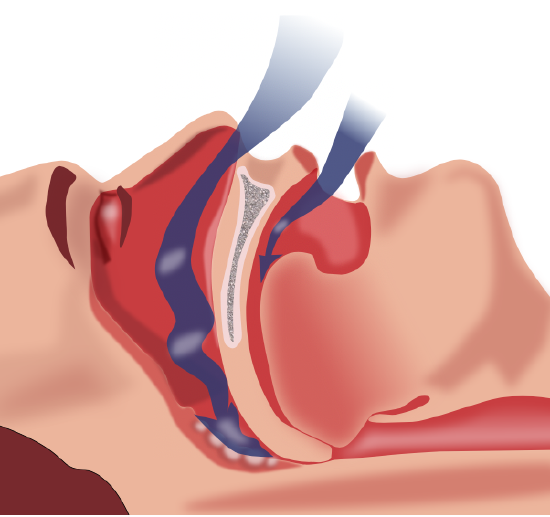
Treatment of sleep apnea may include avoiding alcohol, quitting smoking, or losing weight. Elevating the upper body during sleep or sleeping on one’s side may help prevent airway collapse in many people with sleep apnea. Another type of treatment is the use of an oral device during sleep that shifts the lower jaw forward to help keep the airway open. The most common treatment for moderate to severe sleep apnea is the use during sleep of CPAP (continuous positive airway pressure), which keeps the airway open by means of pressurized air. In this treatment, the person typically wears a plastic facial mask that is connected by a flexible tube to a small bedside CPAP machine. Although CPAP is effective, long-term compliance is often poor because patients find the mask uncomfortable or they experience unpleasant side effects such as dry mouth and nose. A more extreme form of treatment is surgery to remove some of the tissues — such as the tonsils or part of the soft palate — that tend to collapse and block the airway in people with sleep apnea.
Review
- What is asthma, and what are its symptoms and causes?
- Identify common risk factors and triggers of asthma attacks.
- How can asthma attacks be prevented or controlled?
- What are the causes and symptoms of pneumonia?
- How can pneumonia be prevented? How is it treated?
- Define COPD. How is it related to chronic bronchitis and emphysema?
- Relate COPD to tobacco smoking.
- What is the difference between primary and secondary lung cancer?
- What is the major cause of primary lung cancer?
- Discuss lung cancer as a cause of death.
- How is lung cancer treated?
- Define sleep apnea.
- What is the difference between how COPD and pneumonia affect the alveoli?
Explore More
Attributions
- Dust mite by FDA, public domain via Wikimedia Commons
- Asthma attach by United States-National Institute of Health: National Heart, Lung, Blood Institute, public domain via Wikimedia Commons
- New Pneumonia cartoon public domain via Wikimedia Commons
- COPD by National Heart Lung and Blood Institute, public domain via Wikimedia Commons
- Obstruction of ventilation by Habib M’henni via Wikimedia Commons
- Text adapted from Human Biology by CK-12 licensed CC BY-NC 3.0


