13.3: Skin
- Page ID
- 16797
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\( \newcommand{\dsum}{\displaystyle\sum\limits} \)
\( \newcommand{\dint}{\displaystyle\int\limits} \)
\( \newcommand{\dlim}{\displaystyle\lim\limits} \)
\( \newcommand{\id}{\mathrm{id}}\) \( \newcommand{\Span}{\mathrm{span}}\)
( \newcommand{\kernel}{\mathrm{null}\,}\) \( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\) \( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\) \( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\id}{\mathrm{id}}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\kernel}{\mathrm{null}\,}\)
\( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\)
\( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\)
\( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\) \( \newcommand{\AA}{\unicode[.8,0]{x212B}}\)
\( \newcommand{\vectorA}[1]{\vec{#1}} % arrow\)
\( \newcommand{\vectorAt}[1]{\vec{\text{#1}}} % arrow\)
\( \newcommand{\vectorB}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vectorC}[1]{\textbf{#1}} \)
\( \newcommand{\vectorD}[1]{\overrightarrow{#1}} \)
\( \newcommand{\vectorDt}[1]{\overrightarrow{\text{#1}}} \)
\( \newcommand{\vectE}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash{\mathbf {#1}}}} \)
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\(\newcommand{\longvect}{\overrightarrow}\)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\(\newcommand{\avec}{\mathbf a}\) \(\newcommand{\bvec}{\mathbf b}\) \(\newcommand{\cvec}{\mathbf c}\) \(\newcommand{\dvec}{\mathbf d}\) \(\newcommand{\dtil}{\widetilde{\mathbf d}}\) \(\newcommand{\evec}{\mathbf e}\) \(\newcommand{\fvec}{\mathbf f}\) \(\newcommand{\nvec}{\mathbf n}\) \(\newcommand{\pvec}{\mathbf p}\) \(\newcommand{\qvec}{\mathbf q}\) \(\newcommand{\svec}{\mathbf s}\) \(\newcommand{\tvec}{\mathbf t}\) \(\newcommand{\uvec}{\mathbf u}\) \(\newcommand{\vvec}{\mathbf v}\) \(\newcommand{\wvec}{\mathbf w}\) \(\newcommand{\xvec}{\mathbf x}\) \(\newcommand{\yvec}{\mathbf y}\) \(\newcommand{\zvec}{\mathbf z}\) \(\newcommand{\rvec}{\mathbf r}\) \(\newcommand{\mvec}{\mathbf m}\) \(\newcommand{\zerovec}{\mathbf 0}\) \(\newcommand{\onevec}{\mathbf 1}\) \(\newcommand{\real}{\mathbb R}\) \(\newcommand{\twovec}[2]{\left[\begin{array}{r}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\ctwovec}[2]{\left[\begin{array}{c}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\threevec}[3]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\cthreevec}[3]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\fourvec}[4]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\cfourvec}[4]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\fivevec}[5]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\cfivevec}[5]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\mattwo}[4]{\left[\begin{array}{rr}#1 \amp #2 \\ #3 \amp #4 \\ \end{array}\right]}\) \(\newcommand{\laspan}[1]{\text{Span}\{#1\}}\) \(\newcommand{\bcal}{\cal B}\) \(\newcommand{\ccal}{\cal C}\) \(\newcommand{\scal}{\cal S}\) \(\newcommand{\wcal}{\cal W}\) \(\newcommand{\ecal}{\cal E}\) \(\newcommand{\coords}[2]{\left\{#1\right\}_{#2}}\) \(\newcommand{\gray}[1]{\color{gray}{#1}}\) \(\newcommand{\lgray}[1]{\color{lightgray}{#1}}\) \(\newcommand{\rank}{\operatorname{rank}}\) \(\newcommand{\row}{\text{Row}}\) \(\newcommand{\col}{\text{Col}}\) \(\renewcommand{\row}{\text{Row}}\) \(\newcommand{\nul}{\text{Nul}}\) \(\newcommand{\var}{\text{Var}}\) \(\newcommand{\corr}{\text{corr}}\) \(\newcommand{\len}[1]{\left|#1\right|}\) \(\newcommand{\bbar}{\overline{\bvec}}\) \(\newcommand{\bhat}{\widehat{\bvec}}\) \(\newcommand{\bperp}{\bvec^\perp}\) \(\newcommand{\xhat}{\widehat{\xvec}}\) \(\newcommand{\vhat}{\widehat{\vvec}}\) \(\newcommand{\uhat}{\widehat{\uvec}}\) \(\newcommand{\what}{\widehat{\wvec}}\) \(\newcommand{\Sighat}{\widehat{\Sigma}}\) \(\newcommand{\lt}{<}\) \(\newcommand{\gt}{>}\) \(\newcommand{\amp}{&}\) \(\definecolor{fillinmathshade}{gray}{0.9}\)The person in Figure \(\PageIndex{1}\) is no doubt feeling the burn — sunburn that is. Sunburn occurs when the outer layer of the skin is damaged by UV light from the sun or tanning lamps. Some people deliberately allow UV light to burn their skin because after the redness subsides, they are left with a tan. A tan may look healthy, but it is actually a sign of skin damage. People who experience one or more serious sunburns are significantly more likely to develop skin cancer. Natural pigment molecules in the skin help protect it from UV light damage. These pigment molecules are found in the layer of the skin called the epidermis.

The epidermis is the outer of the two main layers of the skin, the inner layer being the dermis. It averages about 0.10 mm thick and is much thinner than the dermis. The epidermis is thinnest on the eyelids (0.05 mm) and thickest on the palms of the hands and soles of the feet (1.50 mm). The epidermis covers almost the entire body surface. It is continuous with, but structurally distinct from, the mucous membranes that line the mouth, anus, urethra, and vagina.
Structure of the Epidermis
There are no blood vessels and very few nerve cells in the epidermis. Without blood to bring epidermal cells oxygen and nutrients, the cells must absorb oxygen directly from the air and obtain nutrients via diffusion of fluids from the dermis below. However, as thin as it is, the epidermis still has a complex structure. It has a variety of cell types and multiple layers.
Cells of the Epidermis
There are several different types of cells in the epidermis. All of the cells are necessary for the important functions of the epidermis.
- The epidermis consists mainly of stacks of keratin-producing epithelial cells called keratinocytes. These cells make up at least 90 percent of the epidermis. Near the top of the epidermis, these cells are also called squamous cells.
- Another 8 percent of epidermal cells are melanocytes. These cells produce the pigment melanin that protects the dermis from UV light.
- About 1 percent of epidermal cells are Langerhans cells. These are immune system cells that detect and fight pathogens entering the skin.
- Less than 1 percent of epidermal cells are Merkel cells, which respond to light touch and connect to nerve endings in the dermis.
Layers of the Epidermis
The epidermis in most parts of the body consists of four distinct layers. A fifth layer occurs in the palms of the hands and soles of the feet, where the epidermis thicker than it is in the rest of the body. The layers of the epidermis are shown in Figure \(\PageIndex{2}\) and described in the following text.
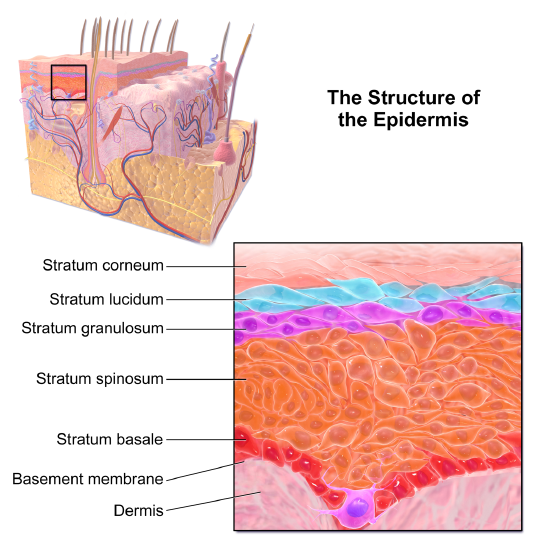
Stratum Basale
The stratum basale is the innermost or the deepest layer of the epidermis. It is separated from the dermis by a membrane called the basement membrane. The stratum basale contains stem cells, called basal cells, which divide to form all the keratinocytes of the epidermis. When keratinocytes first form, they are cube-shaped and contain almost no keratin. As more keratinocytes are produced, previously formed cells are pushed up through the stratum basale. Melanocytes and Merkel cells are also found in the stratum basale. The Merkel cells are especially numerous in touch-sensitive areas such as the fingertips and lips.
Stratum Spinosum
Just above the stratum basale is the stratum spinosum. This is the thickest of the four epidermal layers. The keratinocytes in this layer have begun to accumulate keratin, and they have become tougher and flatter. Spiny cellular projections form between the keratinocytes and hold them together. In addition to keratinocytes, the stratum spinosum contains the immunologically active Langerhans cells.
Stratum Granulosum
The next layer above the stratum spinosum is the stratum granulosum. In this layer, keratinocytes have become nearly filled with keratin, giving their cytoplasm a granular appearance. Lipids are released by keratinocytes in this layer to form a lipid barrier in the epidermis. Cells in this layer have also started to die because they are becoming too far removed from blood vessels in the dermis to receive nutrients. Each dying cell digests its own nucleus and organelles, leaving behind only a tough, keratin-filled shell.
Stratum Lucidum
Only on the palms of the hands and soles of the feet, the next layer above the stratum granulosum is the stratum lucidum. This is a layer consisting of stacks of translucent, dead keratinocytes that provide extra protection to the underlying layers.
Stratum Corneum
The uppermost layer of the epidermis everywhere on the body is the stratum corneum. This layer is made of flat, hard, tightly packed dead keratinocytes that form a waterproof keratin barrier to protect the underlying layers of the epidermis. Dead cells from this layer are constantly shed from the surface of the body. The shed cells are continually replaced by cells moving up from the lower layers of the epidermis. It takes a period of about 48 days for newly formed keratinocytes in the stratum basale to make their way to the top of the stratum corneum to replace shed cells.
Functions of the Epidermis
The epidermis has several crucial functions in the body. These functions include protection, water retention, and vitamin D synthesis.
Protective Functions
The epidermis provides protection to underlying tissues from physical damage, pathogens, and UV light.
Protection from Physical Damage
Most of the physical protection of the epidermis is provided by its tough outer layer, the stratum corneum. Because of this layer, minor scrapes and scratches generally do not cause significant damage to the skin or underlying tissues. Sharp objects and rough surfaces have difficulty penetrating or removing the tough, dead, keratin-filled cells of the stratum corneum. If cells in this layer are pierced or scraped off, they are quickly replaced by new cells moving up to the surface from lower skin layers.
Protection from Pathogens
When pathogens such as viruses and bacteria try to enter the body, it is virtually impossible for them to enter through intact epidermal layers. Generally, pathogens can enter the skin only if the epidermis has been breached, for example by a cut, puncture, or scrape in Figure \(\PageIndex{3}\). That’s why it is important to clean and cover even a minor wound in the epidermis. This helps ensure that pathogens do not use the wound to enter the body. Protection from pathogens is also provided by conditions at or near the skin surface. These include relatively high acidity (pH of about 5.0), low amounts of water, the presence of antimicrobial substances produced by epidermal cells, and Langerhans cells, which phagocytize bacteria or other pathogens.

Protection from UV Light
The UV light that penetrates the epidermis can damage epidermal cells. In particular, it can cause mutations in DNA that lead to the development of skin cancer, in which epidermal cells grow out of control. The UV light can also destroy vitamin B9 (in forms such as folate or folic acid), which is needed for good health and successful reproduction. In a person with light skin, just an hour of exposure to intense sunlight can reduce the body’s vitamin B9 level by 50 percent.
Melanocytes in the stratum basale of the epidermis contain small organelles called melanosomes, which produce, store, and transport the dark brown pigment melanin. As melanosomes become full of melanin, they move into thin extensions of the melanocytes. From there, the melanosomes are transferred to keratinocytes in the epidermis, where they absorb UV light that strikes the skin. This prevents the light from penetrating deeper into the skin and causing damage. The more melanin there is in the skin, the more UV light that can be absorbed.
Water Retention
The ability of the skin to hold water and not lose it to the surrounding environment is due mainly to the stratum corneum. Lipids arranged in an organized way among the cells of the stratum corneum form a barrier to water loss from the epidermis. This is critical for maintaining healthy skin and preserving proper water balance in the body.
Although the skin is impermeable to water, it is not impermeable to all substances. Instead, the skin is selectively permeable, allowing certain fat-soluble substances to pass through the epidermis. The selective permeability of the epidermis is both a benefit and a risk.
- Selective permeability allows certain medications to enter the bloodstream through the capillaries in the dermis. This is the basis of medications that are delivered using topical ointments or patches that are applied to the skin. These include steroid hormones such as estrogen (for hormone replacement therapy), scopolamine (for motion sickness), nitroglycerin (for heart problems), and nicotine (for people trying to quit smoking).
- Selective permeability of the epidermis also allows certain harmful substances to enter the body through the skin. Examples include the heavy metal lead and many pesticides.
Vitamin D Synthesis
Vitamin D is a nutrient that is needed in the human body for the absorption of calcium from food. Molecules of a lipid compound named 7-dehydrocholesterol are precursors of vitamin D. These molecules are present in the stratum basale and stratum spinosum layers of the epidermis. When UV light strikes the molecules, it changes them to vitamin D3. In the kidneys, vitamin D3 is converted to calcitriol, which is the form of vitamin D that is active in the body.
What Gives Skin Its Color?
Melanin in the epidermis is the main substance that determines the color of human skin and explains most of the variation in skin color in people around the world. However, two other substances also contribute to skin color, especially in light-skinned people: carotene and hemoglobin.
- The pigment carotene is present in the epidermis and gives skin a yellowish tint, especially in the skin with low levels of melanin.
- Hemoglobin is a red pigment found in red blood cells. It is visible through the skin as a pinkish tint, again mainly in the skin with low levels of melanin. The pink color is most visible when capillaries in the underlying dermis dilate, allowing greater blood flow near the surface.
Bacteria on Skin
The surface of the human skin normally provides a home to countless numbers of bacteria. Just one square inch of skin normally has an average of about 50 million bacteria. These generally harmless bacteria represent roughly 1,000 bacterial species (Figure \(\PageIndex{4}\)) from 19 different bacterial phyla. Typical variations in the moistness and oiliness of the skin produce a variety of rich and diverse habitats for these microorganisms. For example, the skin in the armpits is warm and moist and often hairy, whereas the skin on the forearms is smooth and dry. These two areas of the human body are as diverse to microorganisms as rainforests and deserts are to larger organisms. The density of bacterial populations on the skin depends largely on the region of the skin and its ecological characteristics. For example, oily surfaces, such as the face, may contain over 500 million bacteria per square inch. Despite the huge number of individual microorganisms living on the skin, their total volume is only about the size of a pea.
In general, the normal microorganisms living on the skin keep one another in check and thereby play an important role in keeping the skin healthy. However, if the balance of microorganisms is disturbed, there may be an overgrowth of certain species, and this may result in an infection. For example, when a patient is prescribed antibiotics, it may kill off normal bacteria and allow an overgrowth of single-celled yeast. Even if the skin is disinfected, no amount of cleaning can remove all of the microorganisms it contains. Disinfected areas are also quickly recolonized by bacteria residing in deeper areas such as hair follicles and in adjacent areas of the skin.
What is Dermis?
The dermis is the inner of the two major layers that make up the skin, the outer layer being the epidermis. The dermis consists mainly of connective tissues. It also contains most skin structures such as glands and blood vessels. The dermis is anchored to the tissues below it by flexible collagen bundles that permit most areas of the skin to move freely over subcutaneous (“below-the-skin”) tissues. Functions of the dermis include cushioning subcutaneous tissues, regulating body temperature, sensing the environment, and excreting wastes.
Anatomy of the Dermis
The basic anatomy of the dermis is a matrix, or sort of scaffolding, composed of connective tissues. These tissues include collagen fibers, which provide toughness; and elastin fibers, which provide elasticity. Surrounding these fibers, the matrix also includes a gel-like substance made of proteins. The tissues of the matrix give the dermis both strength and flexibility.
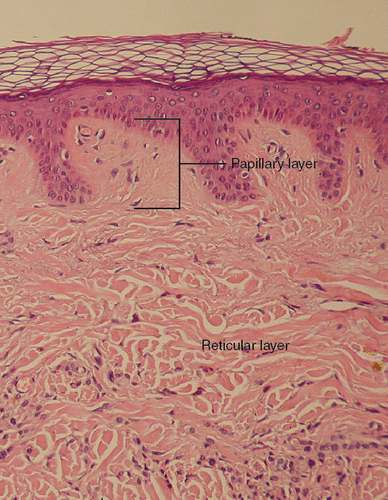
The dermis is divided into two layers: the papillary layer and the reticular layer.
Papillary Layer
The papillary layer is the upper layer of the dermis, just below the basement membrane that connects the dermis to the epidermis above it. The papillary layer is the thinner of the two dermal layers. It is composed mainly of loosely arranged collagen fibers. The papillary layer is named for its fingerlike projections, or papillae, that extend upward into the epidermis. The papillae contain capillaries and sensory touch receptors.
The papillae give the dermis a bumpy surface that interlocks with the epidermis above it, strengthening the connection between the two layers of skin. On the palms and soles, the papillae create epidermal ridges. Epidermal ridges on the fingers are commonly called fingerprints (see the photo below). Fingerprints are genetically determined, so no two people (other than identical twins) have exactly the same fingerprint pattern. Therefore, fingerprints can be used as a means of identification, for example, at crime scenes. Fingerprints were much more commonly used forensically before DNA analysis was introduced for this purpose.

Reticular Layer
The reticular layer is the lower layer of the dermis, below the papillary layer. It is the thicker of the two dermal layers. It is composed of densely woven collagen and elastin fibers. These protein fibers give the dermis its properties of strength and elasticity. This layer of the dermis cushions subcutaneous tissues of the body from stress and strain. The reticular layer of the dermis also contains most of the structures in the dermis, such as glands and hair follicles.
Structures in the Dermis
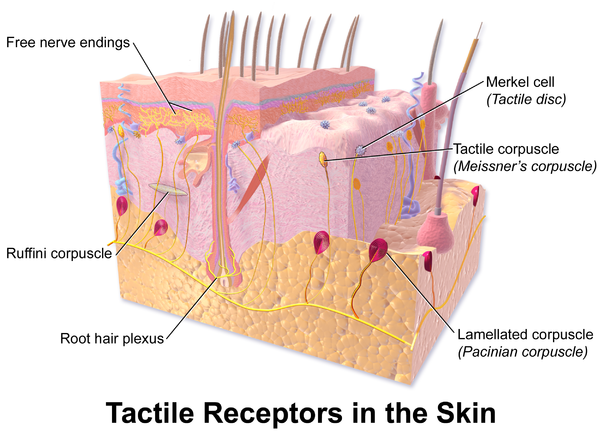
Both papillary and reticular layers of the dermis contain numerous sensory receptors, which make the skin the body’s primary sensory organ for the sense of touch. Both dermal layers also contain blood vessels. They provide nutrients to and remove wastes from dermal cells as well as cells in the lowest layer of the epidermis, the stratum basale. The circulatory components of the dermis are shown in Figure \(\PageIndex{7}\).
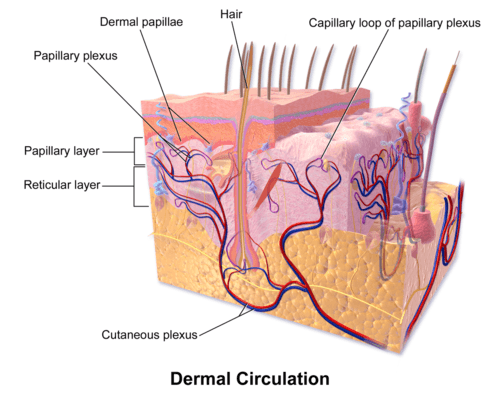
Glands
Glands in the reticular layer of the dermis include sweat glands and sebaceous (oil) glands. Both are exocrine glands, which are glands that release their secretions through ducts to nearby body surfaces. The diagram below shows these glands and also several other structures in the dermis.
Sweat glands produce the fluid called sweat, which contains mainly water and salts. The glands have ducts that carry the sweat to hair follicles or to the surface of the skin. There are two different types of sweat glands: eccrine glands and apocrine glands.
- Eccrine sweat glands occur in the skin all over the body. Their ducts empty through tiny openings called pores onto the skin surface. These sweat glands are involved in temperature regulation.
- Apocrine sweat glands are larger than eccrine glands and occur only in the skin of the armpits and groin. The ducts of apocrine glands empty into hair follicles, and then the sweat travels along hairs to reach the surface. Apocrine glands are inactive until puberty, at which point they start producing an oily sweat that is consumed by bacteria living on the skin. The digestion of apocrine sweat by bacteria is the cause of body odor.
Sebaceous glands are exocrine glands that produce a thick, fatty substance called sebum. Sebum is secreted into hair follicles and makes its way to the skin surface along with hairs. It waterproofs the hair and skin and helps prevent them from drying out. Sebum also has antibacterial properties, so it inhibits the growth of microorganisms on the skin. Sebaceous glands are found in every part of the skin except for the palms of the hands and soles of the feet where hair does not grow.
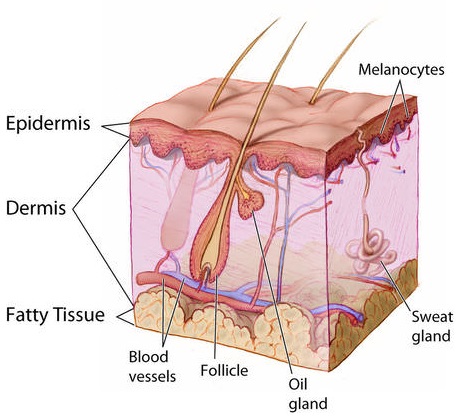
Hair Follicles
Hair follicles are the structures where hairs originate (Figure \(\PageIndex{8}\)). Hairs grow out of follicles, pass through the epidermis, and exit at the surface of the skin. Associated with each hair follicle is a sebaceous gland, which secretes sebum that coats and waterproofs the hair. Each follicle also has a bed of capillaries, a nerve ending, and a tiny muscle called arrector pili.
Functions of the Dermis
The main functions of the dermis are regulating body temperature, enabling the sense of touch, and eliminating wastes from the body.
Temperature Regulation
Several structures in the reticular layer of the dermis are involved in regulating body temperature. For example, when the body temperature rises, the hypothalamus of the brain sends nerve signals to sweat glands, causing them to release sweat. An adult can sweat up to four liters an hour. As the sweat evaporates from the surface of the body, it uses energy in the form of body heat, thus cooling the body. The hypothalamus also causes dilation of blood vessels in the dermis when the body temperature rises. This allows more blood to flow through the skin, bringing body heat to the surface, where it can radiate into the environment.
When the body is too cool, sweat glands stop producing sweat, and blood vessels in the skin constrict, thus conserving body heat. The arrector pili muscles also contract, moving hair follicles and lifting hair shafts. This results in more air being trapped under the hairs to insulate the surface of the skin. These contractions of arrector pili muscles are the cause of goosebumps.
Sensing the Environment
Sensory receptors in the dermis are mainly responsible for the body’s tactile senses. The receptors detect such tactile stimuli as warm or cold temperature, shape, texture, pressure, vibration, and pain. They send nerve impulses to the brain which interprets and responds to the sensory information. Sensory receptors in the dermis can be classified on the basis of the type of touch stimulus they sense. Mechanoreceptors sense mechanical forces such as pressure, roughness, vibration, and stretching. Thermoreceptors sense variations in temperature that are above or below body temperature. Nociceptors sense painful stimuli. Figure \(\PageIndex{9}\) shows several specific kinds of tactile receptors in the dermis. Each kind of receptor senses one or more types of touch stimuli.
- Free nerve endings sense pain and temperature variations.
- Merkel cells sense light touch, shapes, and textures.
- Meissner’s corpuscles sense light touch.
- Pacinian corpuscles sense pressure and vibration.
- Ruffini corpuscles sense stretching and sustained pressure.
Excreting Wastes
The sweat released by eccrine sweat glands is one way the body excretes waste products. Sweat contains excess water, salts (electrolytes), and other waste products that the body must get rid of to maintain homeostasis. The most common electrolytes in sweat are sodium and chloride. Potassium, calcium, and magnesium electrolytes may be excreted in sweat as well. When these electrolytes reach high levels in the blood, extra electrolytes are excreted in sweat. This helps to bring their blood levels back into balance. Besides electrolytes, sweat contains small amounts of waste products from metabolism including ammonia and urea. Sweat may also contain alcohol in someone who has been drinking alcoholic beverages.
Acne is the most common skin disorder in the United States. At least 40 million Americans have acne at any given time. Acne occurs most commonly in teens and young adults, but it can occur at any age. Even newborn babies can get acne.
The main sign of acne is the appearance of pimples (pustules) on the skin, like those in the photo above. Other signs of acne may include whiteheads, blackheads, nodules, and other lesions. Besides the face, acne can appear on the back, chest, neck, shoulders, upper arms, and buttocks. Acne can permanently scar the skin, especially if it isn’t treated appropriately. Besides its physical effects on the skin, acne can also lead to low self-esteem and depression.
Acne is caused by clogged, sebum-filled pores that provide a perfect environment for the growth of bacteria. The bacteria cause infection, and the immune system responds with inflammation. Inflammation, in turn, causes swelling and redness and may be associated with the formation of pus. If the inflammation goes deep into the skin, it may form an acne nodule.
Mild acne often responds well to treatment with over-the-counter (OTC) products containing benzoyl peroxide or salicylic acid. Treatment with these products may take a month or two to clear up the acne. Once the skin clears, treatment generally needs to be continued for some time to prevent future breakouts.
If acne fails to respond to OTC products, nodules develop, or acne is affecting self-esteem, a visit to a dermatologist is in order. A dermatologist can determine which treatment is best for a given patient. A dermatologist can also prescribe prescription medications (which are likely to be more effective than OTC products) and provide other medical treatments such as laser light therapies or chemical peels.
What can you do to maintain healthy skin and prevent or reduce acne? Dermatologists recommend the following tips:
- Wash affected or acne-prone skin (such as the face) twice a day and after sweating.
- Use your fingertips to apply a gentle, non-abrasive cleanser. Avoid scrubbing, which can make acne worse.
- Use only alcohol-free products and avoid any products that irritate the skin, such as harsh astringents or exfoliants.
- Rinse with lukewarm water, and avoid using very hot or cold water.
- Shampoo your hair regularly.
- Do not pick, pop, or squeeze acne. If you do, it will take longer to heal and is more likely to scar.
- Keep your hands off your face. Avoid touching your skin throughout the day.
- Stay out of the sun and tanning beds. Some acne medications make your skin very sensitive to UV light.
Review
- What is the dermis?
- Describe the basic anatomy of the dermis.
- Compare and contrast the papillary and reticular layers of the dermis.
- What causes epidermal ridges, and why can they be used to identify individuals?
- Name the two types of sweat glands in the dermis and state how they differ.
- What is the function of sebaceous glands?
- Describe structures associated with hair follicles.
- Explain how the dermis helps regulate body temperature.
- Identify three specific kinds of tactile receptors in the dermis and the type of stimuli they sense.
- How does the dermis excrete wastes, and what waste products does it excrete?
- What are the subcutaneous tissues? Which layer of the dermis provides cushioning for subcutaneous tissues and why does this layer provide most of the cushioning instead of the other layer?
- For each of the following functions, describe which structure within the dermis carries it out.
- Brings nutrients to and removes wastes from dermal and lower epidermal cells
- Causes hairs to move
- Detects painful stimuli on the skin
- What is the epidermis?
- Identify the types of cells in the epidermis.
- Describe the layers of the epidermis.
- State one function of each of the four epidermal layers found all over the body.
- Explain three ways the epidermis protects the body.
- What makes the skin waterproof?
- Why is the selective permeability of the epidermis both a benefit and risk?
- How is vitamin D synthesized in the epidermis?
- Identify three pigments that impart color to the skin.
- Describe bacteria that normally reside on the skin, and explain why they do not usually cause infections.
- Explain why the keratinocytes at the surface of the epidermis are dead, while keratinocytes located deeper in the epidermis are still alive.
- Which layer of the epidermis contains keratinocytes that have begun to die?
- True or False. The extra layer of epidermis found on the palms of the hands and soles of the feet is located on the very outer surface of the skin.
- True or False. Melanin can be found in keratinocytes.
- Explain why our skin is not permanently damaged if we rub off some of the surface layers by using a rough washcloth.
Explore More
Attributions
- Sunburn by QuinnHK, public domain via Wikimedia Commons
- Structure epidermis by Blausen.com staff (2014). "Medical gallery of Blausen Medical 2014". WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436. licensed CC BY 3.0 via Wikimedia Commons
- Scraped knee by Remux, CC0 via Wikimedia Commons
- Staphylococcus epidermidis by Janice Carr, CDC, public domain via Wikimedia Commons
- Epidermis and dermis slide by Kilbad, public domain via Wikimedia Commons
- Fingerprint detail by Frettie, CC BY 3.0 via Wikimedia Commons
- Dermal circulation by Blausen.com staff (2014). "Medical gallery of Blausen Medical 2014". WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436. licensed CC BY 3.0 via Wikimedia Commons
- Anatomy of the skin by Don Bliss, National Cancer Institute, public domain via Wikimedia Commons
- Skin tactile receptors by Blausen.com staff (2014). "Medical gallery of Blausen Medical 2014". WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436. licensed CC BY 3.0 via Wikimedia Commons
- Text adapted from Human Biology by CK-12 licensed CC BY-NC 3.0


