17.3: Heart
- Page ID
- 92705
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\( \newcommand{\dsum}{\displaystyle\sum\limits} \)
\( \newcommand{\dint}{\displaystyle\int\limits} \)
\( \newcommand{\dlim}{\displaystyle\lim\limits} \)
\( \newcommand{\id}{\mathrm{id}}\) \( \newcommand{\Span}{\mathrm{span}}\)
( \newcommand{\kernel}{\mathrm{null}\,}\) \( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\) \( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\) \( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\id}{\mathrm{id}}\)
\( \newcommand{\Span}{\mathrm{span}}\)
\( \newcommand{\kernel}{\mathrm{null}\,}\)
\( \newcommand{\range}{\mathrm{range}\,}\)
\( \newcommand{\RealPart}{\mathrm{Re}}\)
\( \newcommand{\ImaginaryPart}{\mathrm{Im}}\)
\( \newcommand{\Argument}{\mathrm{Arg}}\)
\( \newcommand{\norm}[1]{\| #1 \|}\)
\( \newcommand{\inner}[2]{\langle #1, #2 \rangle}\)
\( \newcommand{\Span}{\mathrm{span}}\) \( \newcommand{\AA}{\unicode[.8,0]{x212B}}\)
\( \newcommand{\vectorA}[1]{\vec{#1}} % arrow\)
\( \newcommand{\vectorAt}[1]{\vec{\text{#1}}} % arrow\)
\( \newcommand{\vectorB}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\( \newcommand{\vectorC}[1]{\textbf{#1}} \)
\( \newcommand{\vectorD}[1]{\overrightarrow{#1}} \)
\( \newcommand{\vectorDt}[1]{\overrightarrow{\text{#1}}} \)
\( \newcommand{\vectE}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash{\mathbf {#1}}}} \)
\( \newcommand{\vecs}[1]{\overset { \scriptstyle \rightharpoonup} {\mathbf{#1}} } \)
\(\newcommand{\longvect}{\overrightarrow}\)
\( \newcommand{\vecd}[1]{\overset{-\!-\!\rightharpoonup}{\vphantom{a}\smash {#1}}} \)
\(\newcommand{\avec}{\mathbf a}\) \(\newcommand{\bvec}{\mathbf b}\) \(\newcommand{\cvec}{\mathbf c}\) \(\newcommand{\dvec}{\mathbf d}\) \(\newcommand{\dtil}{\widetilde{\mathbf d}}\) \(\newcommand{\evec}{\mathbf e}\) \(\newcommand{\fvec}{\mathbf f}\) \(\newcommand{\nvec}{\mathbf n}\) \(\newcommand{\pvec}{\mathbf p}\) \(\newcommand{\qvec}{\mathbf q}\) \(\newcommand{\svec}{\mathbf s}\) \(\newcommand{\tvec}{\mathbf t}\) \(\newcommand{\uvec}{\mathbf u}\) \(\newcommand{\vvec}{\mathbf v}\) \(\newcommand{\wvec}{\mathbf w}\) \(\newcommand{\xvec}{\mathbf x}\) \(\newcommand{\yvec}{\mathbf y}\) \(\newcommand{\zvec}{\mathbf z}\) \(\newcommand{\rvec}{\mathbf r}\) \(\newcommand{\mvec}{\mathbf m}\) \(\newcommand{\zerovec}{\mathbf 0}\) \(\newcommand{\onevec}{\mathbf 1}\) \(\newcommand{\real}{\mathbb R}\) \(\newcommand{\twovec}[2]{\left[\begin{array}{r}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\ctwovec}[2]{\left[\begin{array}{c}#1 \\ #2 \end{array}\right]}\) \(\newcommand{\threevec}[3]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\cthreevec}[3]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \end{array}\right]}\) \(\newcommand{\fourvec}[4]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\cfourvec}[4]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \end{array}\right]}\) \(\newcommand{\fivevec}[5]{\left[\begin{array}{r}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\cfivevec}[5]{\left[\begin{array}{c}#1 \\ #2 \\ #3 \\ #4 \\ #5 \\ \end{array}\right]}\) \(\newcommand{\mattwo}[4]{\left[\begin{array}{rr}#1 \amp #2 \\ #3 \amp #4 \\ \end{array}\right]}\) \(\newcommand{\laspan}[1]{\text{Span}\{#1\}}\) \(\newcommand{\bcal}{\cal B}\) \(\newcommand{\ccal}{\cal C}\) \(\newcommand{\scal}{\cal S}\) \(\newcommand{\wcal}{\cal W}\) \(\newcommand{\ecal}{\cal E}\) \(\newcommand{\coords}[2]{\left\{#1\right\}_{#2}}\) \(\newcommand{\gray}[1]{\color{gray}{#1}}\) \(\newcommand{\lgray}[1]{\color{lightgray}{#1}}\) \(\newcommand{\rank}{\operatorname{rank}}\) \(\newcommand{\row}{\text{Row}}\) \(\newcommand{\col}{\text{Col}}\) \(\renewcommand{\row}{\text{Row}}\) \(\newcommand{\nul}{\text{Nul}}\) \(\newcommand{\var}{\text{Var}}\) \(\newcommand{\corr}{\text{corr}}\) \(\newcommand{\len}[1]{\left|#1\right|}\) \(\newcommand{\bbar}{\overline{\bvec}}\) \(\newcommand{\bhat}{\widehat{\bvec}}\) \(\newcommand{\bperp}{\bvec^\perp}\) \(\newcommand{\xhat}{\widehat{\xvec}}\) \(\newcommand{\vhat}{\widehat{\vvec}}\) \(\newcommand{\uhat}{\widehat{\uvec}}\) \(\newcommand{\what}{\widehat{\wvec}}\) \(\newcommand{\Sighat}{\widehat{\Sigma}}\) \(\newcommand{\lt}{<}\) \(\newcommand{\gt}{>}\) \(\newcommand{\amp}{&}\) \(\definecolor{fillinmathshade}{gray}{0.9}\)Lub dub, lub dub, lub dub... That’s how the sound of a beating heart is typically described. In a normal, healthy heart, those are the only two sounds that should be audible when listening to the heart through a stethoscope. If a physician assistant hears something different from the normal lub dub sounds, it’s a sign of a possible heart abnormality. What causes the heart to produce the characteristic lub dub sounds? Read on to find out.

The heart is a muscular organ behind the sternum (breastbone), slightly to the left of the center of the chest. A normal adult heart is about the size of a fist. The function of the heart is to pump blood through the blood vessels of the cardiovascular system. The continuous flow of blood through the system is necessary to provide all the cells of the body with oxygen and nutrients and to remove their metabolic wastes.
Structure of the Heart
The heart has a thick muscular wall that consists of several layers of tissue. Internally, the heart is divided into four chambers through which blood flows. Blood flows in just one direction through the chambers due to heart valves.
Heart Wall
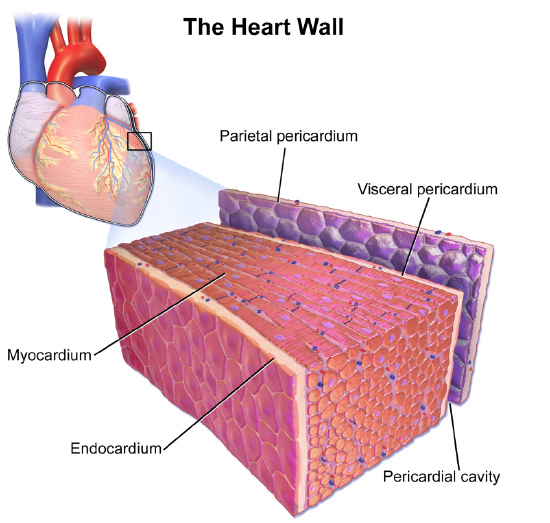
As shown in Figure \(\PageIndex{2}\), the wall of the heart is made up of three layers, called the endocardium, myocardium, and pericardium.
- The endocardium is the innermost layer of the heart wall. It is made up primarily of simple epithelial cells. It covers the heart chambers and valves. A thin layer of connective tissue joins the endocardium to the myocardium.
- The myocardium is the middle and thickest layer of the heart wall. It consists of cardiac muscle surrounded by a framework of collagen. There are two types of cardiac muscle cells in the myocardium: pacemaker cells, which have the ability to contract easily; and pacemaker cells, which conduct electrical impulses that cause the cardiomyocytes to contract. About 99 percent of cardiac muscle cells are cardiomyocytes, and the remaining 1 percent are pacemaker cells. The myocardium is supplied with blood vessels and nerve fibers via the pericardium.
- The epicardium is the third layer which is a part of the pericardium, a protective sac that encloses and protects the heart. The pericardium consists of two membranes (visceral pericardium called epicardium and parietal pericardium), between which there is a fluid-filled cavity. The fluid helps to cushion the heart and also lubricates its outer surface.
Heart Chambers
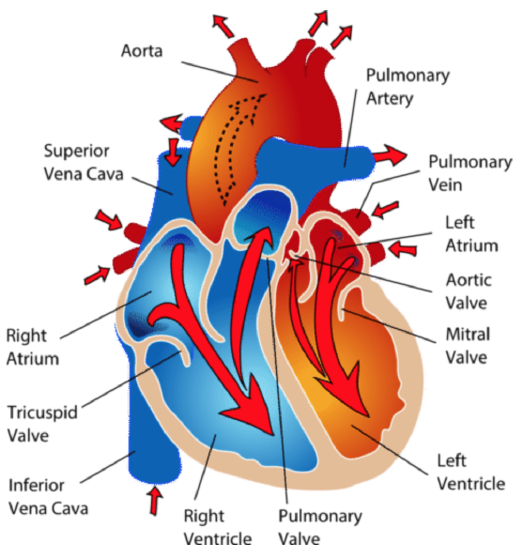
As shown in Figure \(\PageIndex{3}\), the four chambers of the heart include two upper chambers called atria (singular, atrium) and two lower chambers called ventricles. The atria are also referred to as receiving chambers because blood coming into the heart first enters these two chambers. The right atrium receives blood from the upper and lower body through the superior vena cava and inferior vena cava, respectively; and the left atrium receives blood from the lungs through the pulmonary veins. The ventricles are also referred to as discharging chambers because the blood leaving the heart passes out through these two chambers. The right ventricle discharges blood to the lungs through the pulmonary artery, and the left ventricle discharges blood to the rest of the body through the aorta. The four chambers are separated from each other by dense connective tissue consisting mainly of collagen.
Heart Valves
Figure \(\PageIndex{3}\) also shows the location of the four valves of the heart. The heart valves allow blood to flow from the atria to the ventricles and from the ventricles to the pulmonary artery and aorta. The valves are constructed in such a way that blood can flow through them in only one direction, thus preventing the backflow of blood. The four valves are the:
- tricuspid valve, which allows blood to flow from the right atrium to the right ventricle.
- the mitral valve, which allows blood to flow from the left atrium to the left ventricle.
- pulmonary valve, which allows blood to flow from the right ventricle to the pulmonary artery.
- the aortic valve, which allows blood to flow from the left ventricle to the aorta.
The tricuspid and mitral valves are also called atrioventricular (or AV) valves because they are found between the atrium and the ventricle. The pulmonary and aortic valves are also called semilunar valves because they are shaped like half-moons.
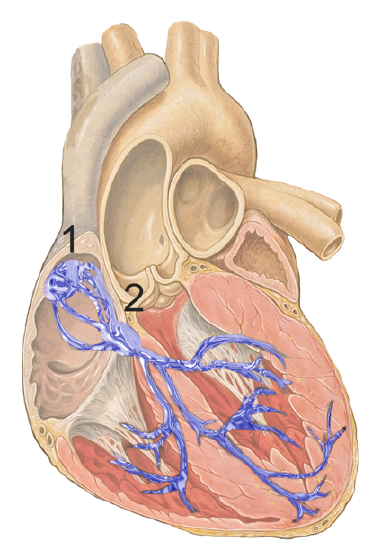
Coronary Circulation
The cardiomyocytes of the muscular walls of the heart are very active cells because they are responsible for the constant beating of the heart. These cells need a continuous supply of oxygen and nutrients. The carbon dioxide and waste products they produce also must be continuously removed. The blood vessels that carry blood to and from the heart muscle cells make up the coronary circulation. Note that the blood vessels of the coronary circulation supply heart tissues with blood and are different from the blood vessels that carry blood to and from the chambers of the heart as part of the general circulation. Coronary arteries supply oxygen-rich blood to the heart muscle cells. Coronary veins remove deoxygenated blood from the heart muscle cells.
- There are two coronary arteries: a right coronary artery that supplies the right side of the heart and a left coronary artery that supplies the left side of the heart. These arteries branch repeatedly into smaller and smaller arteries and finally into capillaries, which exchange gases, nutrients, and waste products with cardiomyocytes.
- At the back of the heart, small cardiac veins drain into larger veins and finally into the great cardiac vein, which empties into the right atrium. At the front of the heart, small cardiac veins drain directly into the right atrium.
Blood Circulation Through the Heart
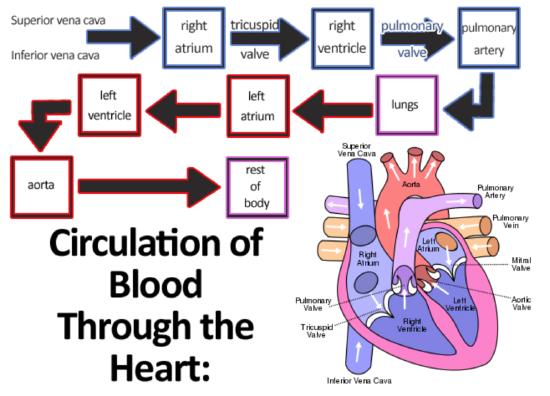
Figure \(\PageIndex{4}\) shows how blood circulates through the chambers of the heart. The right atrium collects blood from two large veins, the superior vena cava (from the upper body) and the inferior vena cava (from the lower body). The blood that collects in the right atrium is pumped through the tricuspid valve into the right ventricle. From the right ventricle, the blood is pumped through the pulmonary valve into the pulmonary artery. The pulmonary artery carries the blood to the lungs, where it enters the pulmonary circulation, gives up carbon dioxide, and picks up oxygen. The oxygenated blood travels back from the lungs through the pulmonary veins (of which there are four) and enters the left atrium of the heart. From the left atrium, the blood is pumped through the mitral valve into the left ventricle. From the left ventricle, the blood is pumped through the aortic valve into the aorta, which subsequently branches into smaller arteries that carry the blood throughout the rest of the body. After passing through capillaries and exchanging substances with cells, the blood returns to the right atrium via the superior vena cava and inferior vena cava, and the process begins anew.
Cardiac Cycle
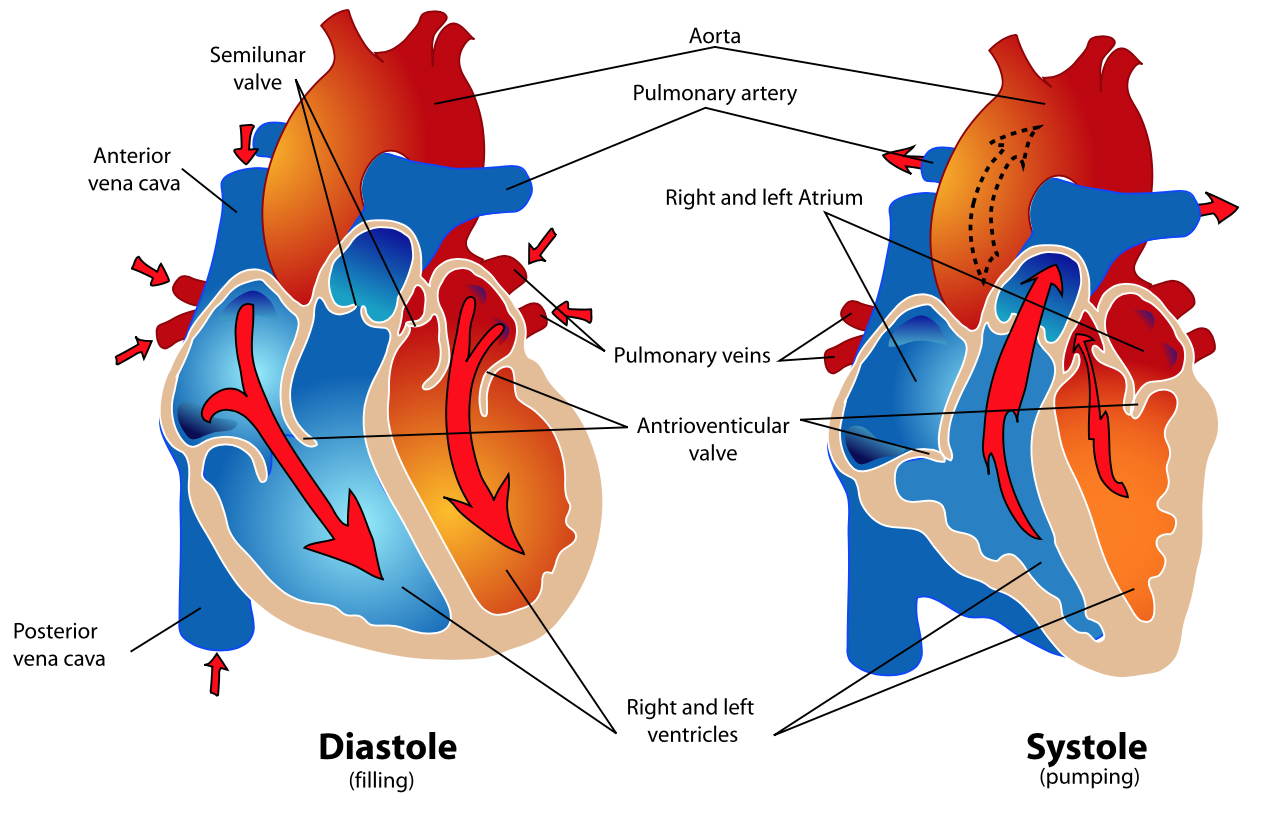
The cardiac cycle refers to a single complete heartbeat, which includes one iteration of the lub and dub sounds heard through a stethoscope. During the cardiac cycle, the atria and ventricles work in a coordinated fashion so that blood is pumped efficiently through and out of the heart. The cardiac cycle includes two parts, called diastole and systole, which are illustrated in Figure \(\PageIndex{5}\).
- During diastole, the atria contract and pump blood into the ventricles, while the ventricles relax and fill with blood from the atria.
- During systole, the atria relax and collect blood from the lungs and body, while the ventricles contract and pump blood out of the heart.
Electrical Stimulation of the Heart
The normal, rhythmical beating of the heart is called sinus rhythm. It is established by the heart’s pacemaker cells, which are located in an area of the heart called the sinoatrial node (Figure \(\PageIndex{6}\)). The pacemaker cells create electrical signals by the movement of electrolytes (sodium, potassium, and calcium ions) into and out of the cells. For each cardiac cycle, an electrical signal rapidly travels first from the sinoatrial node to the right and left atria so they contract together. Then the signal travels to another node, called the atrioventricular node (also shown in Figure \(\PageIndex{6}\)), and from there to the right and left ventricles, which also contract together, just a split second after the atria contract.
The normal sinus rhythm of the heart is influenced by the autonomic nervous system through sympathetic and parasympathetic nerves. These nerves arise from two paired cardiovascular centers in the medulla of the brainstem. The parasympathetic nerves act to decrease the heart rate, and the sympathetic nerves act to increase the heart rate. Parasympathetic input normally predominates. Without it, the pacemaker cells of the heart would generate a resting heart rate of about 100 beats per minute, instead of a normal resting heart rate of about 72 beats per minute. The cardiovascular centers receive input from receptors throughout the body and act through the sympathetic nerves to increase the heart rate as needed. For example, increased physical activity is detected by receptors in muscles, joints, and tendons. These receptors send nerve impulses to the cardiovascular centers, causing sympathetic nerves to increase the heart rate. This allows more blood to flow to the muscles.
Besides the autonomic nervous system, other factors can also affect the heart rate. For example, thyroid hormones and adrenal hormones such as epinephrine can stimulate the heart to beat faster. The heart rate also increases when blood pressure drops or the body is dehydrated or overheated. On the other hand, cooling of the body and relaxation, among other factors, can contribute to a decrease in the heart rate.
Feature: Human Biology in the News
When a patient’s heart is too diseased or damaged to sustain life, a heart transplant is likely to be the only long-term solution. The first successful heart transplant was undertaken in South Africa in 1967. For the past two decades in the United States, about 2,400 hearts were transplanted each year. The problem is that far too few hearts are available for transplant, and many patients die each year waiting for a life-saving heart to become available.
Hearts for transplant have to be used within four hours of the death of the donor. In addition, hearts can only come from brain-dead individuals whose hearts are removed while they are still healthy. Then the hearts are placed on ice inside picnic coolers to be transported to a waiting recipient. The four-hour window means that traffic jams, bad weather, or other unforeseen delays often result in a heart being in less than optimal condition by the time it arrives at its destination. Unfortunately, there is no way to know if the heart will start up again after it is transplanted until it is actually placed in the recipient’s body. In up to seven percent of cases, a transplanted heart does not work and has to be removed.
A medical device company in Massachusetts named TransMedic was featured in many news stories when it developed the Organ Care System, commonly referred to as “heart in a box.” The system takes a new approach to maintain donated hearts until they are transplanted. The box is heated and contains a device that pumps oxygenated blood through the heart while it is being transported to the recipient. This extends the time up to 12 hours that the heart can remain healthy and usable. It also allows the heart to be monitored so it is kept in optimal condition while it is on the route. The end result, ideally, is that the recipient gets a healthier heart with less chance of failure of the new organ and a lower risk of death.
As of mid-2016, the heart-in-a-box system had already been used for several successful heart transplants in other countries. At that time, the system was also undergoing clinical trials in the United States to assess its effectiveness in promoting positive recipient outcomes. Developers of the heart-in-a-box predict that the system could increase the number of usable donor hearts by as much as 30 percent, thus greatly increasing the number of patients who are saved from death due to heart failure.
Review
- What is the heart, where is located, and what is its function?
- Outline the structure of the heart.
- Describe the coronary circulation.
- Summarize how blood flows into, through, and out of the heart.
- Define the cardiac cycle, and identify its two parts.
- Explain what controls the beating of the heart.
- a. What are the two types of cardiac muscle cells in the myocardium?
b. What are the differences between these two types of cells?
- Match each of the three layers of the walls of the heart (endocardium, myocardium, and pericardium) with the description that best matches it below.
a. Protects the heart
b. Covers the heart valves
c. Responsible for the beating of the heart
- Is the blood flowing through the mitral valve oxygenated or deoxygenated? Explain your reasoning.
- True or False. The coronary arteries carry blood to the heart.
- True or False. Systole is when the heart is contracting, diastole is when the heart is fully relaxed.
- Explain why the blood from the cardiac veins empties into the right atrium of the heart. Focus on function rather than anatomy in your answer.
Explore More
More women than men die of heart disease, but heart research has long focused on men. In the following TED talk, pioneering doctor C. Noel Bairey Merz shares what we know and don't know about women's heart health, including the very different heart attack symptoms women experience and why doctors often miss them.
Attributions
- "MEDCAP - Natural Fire 10 - Palabek Kal Health Clinic - US Army Africa - AFRICOM - 091018-F-8314S-229" by US Army Africa is licensed under CC BY 2.0 via Flickr
- Heart Wall by Blausen.com staff (2014). "Medical gallery of Blausen Medical 2014". WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436. licensed CC BY 3.0 via Wikimedia Commons.
- Heart by CK-12 licensed CC BY-NC 3.0
- Circulation of Blood Through the Heart by Emibitch, public domain via Wikimedia Commons
- Human healthy pumping heart by Mariana Ruiz Villarreal (LadyofHats), public domain via Wikimedia Commons
- Heart conduction system by J. Heuser, CC BY 2.5 via Wikimedia Commons
- Text adapted from Human Biology by CK-12 licensed CC BY-NC 3.0


