6.1A: Overall Mechanism
- Page ID
- 3196
Define cytokine and chemokine and name 3 inflammatory cytokines. State the mechanism forinflammation and state why it is primarily beneficial to the body. Briefly describe why inflammation during a minor or moderate infection is essentially beneficial while inflammation during a massive infection can cause considerable damage to the body. Looking at the overall mechanism behind septic shock, answer the following: - Describe how bacterial PAMPS initiate SIRS.
- Define hypotension and describe the biological mechanism behind 3 factors that contribute to hypotension.
- Define hypovolemia and describe the biological mechanism behind 3 factors that contribute to hypovolemia.
- Define hypoperfusion and describe the biological mechanism behind at least 3 factors that contribute to hypoperfusion.
- Describe the biological mechanism behind ARDS and how ARDS contributes to hypoperfusion.
- Describe the sequence of events that enables hypoperfusion to lead to irreversible cell damage.
Define pyroptosis and inflammasome and state their role in inducing inflammation. Define the following: - vasodilation
- septicemia
- hypotension
- hypovolemia
- septic shock
- DIC
- ARDS
- MOSF
- hypoperfusion
- Describe how bacterial PAMPS initiate SIRS.
- Define hypotension and describe the biological mechanism behind 3 factors that contribute to hypotension.
- Define hypovolemia and describe the biological mechanism behind 3 factors that contribute to hypovolemia.
- Define hypoperfusion and describe the biological mechanism behind at least 3 factors that contribute to hypoperfusion.
- Describe the biological mechanism behind ARDS and how ARDS contributes to hypoperfusion.
- Describe the sequence of events that enables hypoperfusion to lead to irreversible cell damage.
- vasodilation
- septicemia
- hypotension
- hypovolemia
- septic shock
- DIC
- ARDS
- MOSF
- hypoperfusion
The binding of PAMPs to PRRs also leads to activation of the complement pathways and activation of the coagulation pathway.
Cytokines such as tumor necrosis factor-alpha (TNF-alpha), interleukin-1 (IL-1), and interleukin-8 (IL-8) are known as inflammatory cytokines because they promote inflammation. Some cytokines, such as IL-8, are also known as chemokines. Chemokines promote an inflammatory response by enabling white blood cells to leave the blood vessels and enter the surrounding tissue, by chemotactically attracting these white blood cells to the infection site, and by triggering neutrophils to release killing agents for extracellular killing.
Inflammation is the first response to infection and injury and is critical to body defense. Basically, the inflammatory response is an attempt by the body to restore and maintain homeostasis after injury. Most of the body defense elements are located in the blood, and inflammation is the means by which body defense cells and defense chemicals leave the blood and enter the tissue around an injured or infected site. The release of inflammatory cytokines eventually leads to vasodilation of blood vessels. Vasodilation is a reversible opening of the junctional zones between endothelial cells of the blood vessels and results in increased blood vessel permeability. This enables plasma, the liquid portion of the blood, to enter the surrounding tissue. The plasma contains defense chemicals such as antibody molecules, complement proteins, lysozyme, and human defensins. Increased capillary permeability also enables white blood cells to squeeze out of the blood vessels and enter the tissue. As can be seen, inflammation is necessary part of body defense. Excessive or prolonged inflammation can, however, cause harm as will be discussed below.
(Scanning electron micrographs of a cross section of a capillary showing an endothelial cell and a capillary with a red blood cell; courtesy of Dennis Kunkel's Microscopy.)
As mentioned in a previous section, products of the complement pathways lead to: 1)more inflammation; 2) opsonization of bacteria; 3) chemotaxis of phagocytes to the infected site; and 4) MAC lysis of gram-negative bacteria.
The products of the coagulation pathway lead to the clotting of blood to stop bleeding, more inflammation, and localization of infection.
At moderate levels, inflammation, products of the complement pathways, and products of the coagulation pathway are essential to body defense. However, these same processes and products when excessive can cause considerable harm to the body.
During minor local infections with few bacteria present, low levels of PAMPs are released leading to moderate cytokine production by defense cells such as monocytes, macrophages, and dendritic cells and, in general, promoting body defense by stimulating inflammation and moderate fever, breaking down energy reserves to supply energy for defense, activating the complement pathway and the coagulation pathway, and generally stimulating immune responses (see Figure \(\PageIndex{2}\)). Also as a result of these cytokines, circulating phagocytic white blood cells such as neutrophils and monocytes stick to the walls of capillaries, squeeze out and enter the tissue, a process termed diapedesis. The phagocytic white blood cells such as neutrophils then kill the invading microbes with their proteases and toxic oxygen radicals. These defenses will be covered in greater detail in Units 5 and 6.
However, during severe systemic infections with large numbers of bacteria present, high levels of PAMPs are released resulting in excessive cytokine production by the defense cells and this can harm the body (see Figure \(\PageIndex{3}\)). In addition, neutrophils start releasing their proteases and toxic oxygen radicals that kill not only the bacteria, but the surrounding tissue as well. Harmful effects include high fever, hypotension, tissue destruction, wasting, acute respiratory distress syndrome (ARDS), disseminated intravascular coagulation (DIC), and damage to the vascular endothelium. This can result in shock, multiple system organ failure (MSOF), and death.
| YouTube animation illustrating macrophages releasing cytokines. Nucleus Medical Art, www. nucleusinc.com |
Sepsis and Systemic Inflammatory Response Syndrome (SIRS)
Keep in mind that a primary function of the circulatory system is perfusion, the delivery of nutrients and oxygen via arterial blood to a capillary bed in tissue. This, in turn, delivers nutrients for cellular metabolism and oxygen for energy production via aerobic respiration to all of the cells of the body. Sepsis is an infection that leads to a systemic inflammatory response resulting in physiologic changes occurring at the capillary endothelial level. This systemic inflammatory response is referred to as Systemic Inflammatory Response Syndrome or SIRS.
Based on severity, there are three sepsis syndromes based on severity:
1. Sepsis. SIRS in the setting of an infection.
2. Severe sepsis. An infection with end-organ dysfunction as a result of hypoperfusion, the reduced delivery of nutrients and oxygen to tissues and organs via the blood.
3. Septic shock. Severe sepsis with persistent hypotension and tissue hypoperfusion despite fluid resuscitation.
We will now take a look at the underlying mechanism of SIRS that can result in septic shock.
Systemic Inflammatory Response Syndrome (SIRS) Resulting in Septic Shock
During a severe systemic infection, an excessive inflammatory response triggered by overproduction of inflammatory cytokines such as TNF-alpha, IL-1, IL-6, IL-8, and PAF in response to PAMPs often occurs.
The release of inflammatory cytokines eventually leads to vasodilation of blood vessels. Vasodilation is a reversible opening of the junctional zones between endothelial cells of the blood vessels and results in increased blood vessel permeability. Normally, this fights the infection by enabling plasma, the liquid portion of the blood, to enter the surrounding tissue. The plasma contains defense chemicals such as antibody molecules, complement proteins, lysozyme, and human defensins. Increased capillary permeability also enables white blood cells to adhere to the inner capillary wall, squeeze out of the blood vessels, and enter the tissue to fight infection, a process called diapedesis.
Excessive productions of cytokines during a systemic infection results in the following events:
1. During diapedesis, phagocytic WBCs called neutrophils adhere to capillary walls in massive amounts. Chemokines such as IL-8 activate extracellular killing by neutrophils, causing them to release proteases and toxic oxygen radicals while still in the capillaries. These are the same toxic chemicals neutrophils use to kill microbes, but now they are dumped onto the vascular endothelial cells to which the neutrophils have adhered.
a. This results in damage to the capillary walls and leakage of blood into surrounding tissue (see Figure \(\PageIndex{4}\)).
b. Blood leakage, in turn, can result in hypovolemia, a decreased volume of circulating blood. (Bleeding from physical trauma, internal bleeding, insufficient rehydration, and loss of fluids from vomiting and diarrhea can also lead to hypovolemia.)
c. Hypovolemia then contributes to hypotension, or low blood pressure.
d. Hypotension then contributes to hypoperfusion.
2. Prolonged vasodilation and the resulting increased capillary permeability causes plasma to leave the bloodstream and enter the tissue.
a. This too contributes to a decreased volume of circulating blood or hypovolemia.
b. Hypovolemia then contributes to hypotension.
c. Hypotension then contributes to hypoperfusion def).
Prolonged vasodilation also leads to decreased vascular resistance within blood vessels.
a. The lower the vascular resistance, the lower the blood pressure. This too contributes to a drop in blood pressure or hypotension.
b. Hypotension then contributes to hypoperfusion.
3. At high levels of TNF, vascular smooth muscle tone and myocardial contractility are inhibited.
a. Decreased myocardial contractility results in a marked hypotension.
b. Hypotension then contributes to hypoperfusion.
c. Cytokine-induced overproduction of nitric oxide (NO) by cardiac muscle cells and vascular smooth muscle cells can also lead to heart failure.
4. Activation of the blood coagulation pathway can cause clots called microthrombi to form within the blood vessels throughout the body. This is called disseminated intravascular coagulation (DIC).
a. These microthrombi physically block the capillaries and contributes to hypoperfusion.
b. Activation of neutrophils also leads to their accumulation and plugging of the vasculature.
c. Depletion of clotting factors as a result of DIC leads to hemorrhaging in many parts of the body following the neutrophil-induced capillary damage. This, as mentioned above, contributes to a decreased volume of circulating blood or hypovolemia.
d. Hypovolemia then contributes to hypotension.
e. Hypotension then contributes to hypoperfusion.
5. In the lungs, the increased capillary permeability as a result of inflammation and vasodilation, as well as neutrophil-induced injury to capillaries in the alveoli leads to pulmonary edema. As the alveoli fill with fluid gas exchange does not occur in the lungs. This condition is called acute respiratory distress syndrome (ARDS).
a. As a result, the blood does not become oxygenated.
b. Lack of oxygenation of the blood via the lungs then causes hypoperfusion.
6. Hypoperfusion and capillary damage In the liver results in impaired liver function and a failure to maintain normal blood glucose levels.
Overuse of glucose by muscles and a failure of the liver to replace glucose can lead to a drop in blood glucose level below what is needed to sustain life. (Glucose is needed to make ATP via aerobic respiration.)
7. Hypoperfusion in the kidneys, bowels, or brain can lead to injury of these organs.
8. The combination of hypotension, hypovolemia, DIC, ARDS, and the resulting hypoperfusion then leads to acidosis.
a. Without oxygen, cells switch to fermentation and produce lactic acid that lowers the pH of the blood. A blood pH range between 6.8 and 7.8 is needed for normal cellular enzyme activity in humans.
b. Changes in the pH of arterial blood extracellular fluid outside this range lead to irreversible cell damage.
In summary, the release of excessive levels of inflammatory cytokines in response to PAMPs binding to PRRs during a systemic infection results in:
1. A drop in blood volume or hypovolemia. This is caused by the following events:
a. Extracellular killing by neutrophils damages the capillary walls results in blood and plasma leaving the bloodstream and entering the surrounding tissue.
b. Depletion of clotting factors during disseminated intravascular coagulation (DIC) can lead to hemorrhaging as the capillaries are damaged.
c. Prolonged vasodilation results in plasma leaving the bloodstream and entering the surrounding tissue.
2. A drop in blood pressure or hypotension. This is a result of the following events:
a. Prolonged vasodilation causes decreased vascular resistance within blood vessels decreases blood pressure.
b. High levels of TNF, inhibit vascular smooth muscle tone and myocardial contractility decreasing the ability of the heart to pump blood throughout the body.
c. Hypovolemia from capillary damage, plasma leakage, and hemorrhaging.
3. The inability to deliver nutrients and oxygen to body cells or hypoperfusion. This is a result of the following events:
a. Activation of the blood coagulation pathway can cause clots called microthrombi to form within the blood vessels throughout the body causing disseminated intravascular coagulation (DIC) which blocks the flow of blood through the capillaries and, as mentioned above, depletion of clotting factors can lead to hemorrhaging in many parts of the body.
b. Increased capillary permeability as a result of vasodilation in the lungs, as well as neutrophil-induced injury to capillaries in the alveoli leads to acute inflammation, pulmonary edema, and loss of gas exchange in the lungs (acute respiratory distress syndrome or ARDS). As a result, the blood does not become oxygenated.
c. Hypovolemia decreases the volume of circulating blood and leads to hypotension.
d. Hypotension decreases the pressure needed to deliver blood throughout the body.
6. Hypoperfusion in the liver can result in a drop in blood glucose level from liver dysfunction. Glucose is needed for ATP production during glycolysis and aerobic respiration. A drop in glucose levels can result in decreased ATP production and insufficient energy for cellular metabolism.
7. The lack of oxygen delivery as a result of hypoperfusion causes cells to switch to fermentation for energy production. The acid end products of fermentation lead to acidosis and the wrong pH for the functioning of the enzymes involved in cellular metabolism. This can result in irreversible cell death.
Collectively, this can result in :
- End-organ ischemia Ischemia is a restriction in blood supply that results in damage or dysfunction of tissues or organs.
- Multiple system organ failure (MSOF). Multiple organs begin to fail as a result of hypoperfusion.
- Death.
For more on SIRS and Septic Shock, see Septic Shock.
| Concept map for SIRS and Septic Shock. |
Define hypotension and describe the biological mechanism behind 2 factors that contribute to hypotension. Define hypovolemia and describe the biological mechanism behind 3 factors that contribute to hypovolemia. Define hypoperfusion and describe the biological mechanism behind 3 factors that contribute to hypoperfusion. Describe the biological mechanism behind ARDS and how ARDS contributes to hypoperfusion. Describe the sequence of events that enables hypoperfusion to lead to irreversible cell damage. What is end-organ ischemia?
Septicemia is a condition where bacteria enter the blood and cause harm. According to the NIH Sepsis Fact Sheet, “Every year, severe sepsis strikes about 750,000 Americans. It’s been estimated that between 28 and 50 percent of these people die - far more than the number of U.S. deaths from prostate cancer, breast cancer and AIDS combined.” Factors contributing to this high rate of sepsis include:
1. An aging US population.
2. Increased longevity of people with chronic diseases.
3. An increase in number of invasive medical procedures performed.
4. Increased use of immunosuppressive and chemotherapeutic agents.
5. The spread of antibiotic-resistant microorganisms.
People that survive severe sepsis may have permanent damage to the lungs or other organs. Approximately 45% of the cases of septicemia are due to Gram-positive bacteria, 45% are a result of Gram-negative bacteria, and 10% are due to fungi (mainly the yeast Candida). Many of these cases of septicemia are health care-associated infections (HA Is).
The Centers for Disease Control and Prevention (CDC) Health care-associated infection's website reports that "In American hospitals alone, health care-associated infections account for an estimated 1.7 million infections and 99,000 associated deaths each year. Of these infections:
- 32 percent of all health care-associated infection are urinary tract infections
- 22 percent are surgical site infections
- 15 percent are pneumonia (lung infections)
- 14 percent are bloodstream infections"
| Estimates of Health care-Associated Infections (HCIs) 2011; from CDC |
We will now look at various bacterial PAMPs that lead to cytokine production, inflammation, and activation of the complement and coagulation pathways.
Summary
- In order to protect against infection, one of the things the body must initially do is detect the presence of microorganisms.
- The body does this by recognizing molecules unique to microorganisms that are not associated with human cells. These unique molecules are called pathogen-associated molecular patterns or PAMPs.
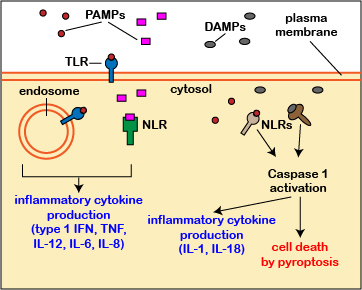
- PAMPS bind to pattern-recognition receptors (PRRs) on defense cells which lead to the production of cytokines that trigger inflammation, activate the complement pathways, and activate the coagulation pathway. This inflammatory response is accomplished primarily by an inflammatory programmed cell death called pyroptosis involving protein cellular complexes called inflammasomes.
- Cytokines such as tumor necrosis factor-alpha (TNF-alpha), interleukin-1 (IL-1), interleukin-6 (IL-6), and interleukin-8 (IL-8) are known as inflammatory cytokines because they promote inflammation.
- Inflammation is the means by which body defense cells and defense chemicals leave the blood and enter the tissue around an injured or infected site.
- Vasodilation is a reversible opening of the junctional zones between endothelial cells of the blood vessels and results in increased blood vessel permeability. This enables plasma, the liquid portion of the blood, to enter the surrounding tissue. Increased capillary permeability also enables white blood cells to squeeze out of the blood vessels and enter the tissue.
- When there is a minor infection with few bacteria present, low levels of PAMPs are present. This leads to moderate cytokine production by defense cells and, in general, promotes body defense.
- During severe systemic infections with large numbers of bacteria present, high levels of PAMPs are released resulting in excessive cytokine production by the defense cells and this can harm the body.
- Perfusion refers to the delivery of nutrients and oxygen via arterial blood to a capillary bed in tissue.
- Sepsis is an infection that leads to a systemic inflammatory response resulting in physiologic changes occurring at the capillary endothelial level. This systemic inflammatory response is referred to as Systemic Inflammatory Response Syndrome or SIRS.
- Cytokine-induced extracellular killing by neutrophils adhere to capillary walls results in damage to the capillary walls and leakage of blood into surrounding tissue. This contributes to a decreased volume of circulating blood (hypovolemia).
- Prolonged vasodilation and the resulting increased capillary permeability causes plasma to leave the bloodstream and enter the tissue. This contributes to a decreased volume of circulating blood (hypovolemia).
- Prolonged vasodilation also leads to decreased vascular resistance within blood vessels resulting in a drop in blood pressure (hypotension).
- At high levels of TNF, vascular smooth muscle tone and myocardial contractility are inhibited. This results in a marked hypotension.
- Hypovolemia as a result of hemorrhaging, systemic edema, insufficient hydration, or loss of fluids through vomiting and diarrhea also leads to hypotension.
- Activation of the blood coagulation pathway can cause clots called microthrombi to form within the blood vessels throughout the body (disseminated intravascular coagulation or DIC). These microthrombi block the capillaries. Depletion of clotting factors leads to hemorrhaging in many parts of the body following neutrophil-induced capillary damage.
- Increased capillary permeability as a result of vasodilation in the lungs, as well as neutrophil-induced injury to capillaries in the alveoli leads to acute inflammation, pulmonary edema, and loss of gas exchange in the lungs (acute respiratory distress syndrome or ARDS). As a result, the blood does not become oxygenated.
- The combination of hypotension, hypovolemia, DIC, ARDS, results in hypoperfusion.
- Without oxygen, cells switch to fermentation and produce lactic acid that lowers the pH of the blood (acidosis). A blood pH range between 6.8 and 7.8 is needed for normal cellular enzyme activity in humans. Changes in the pH of arterial blood extracellular fluid outside this range lead to irreversible cell damage.
- Collectively, this can result in end-organ ischemia (a restriction in blood supply that results in damage or dysfunction of tissues or organs), multiple system organ failure (MSOF), and death.
- According to the NIH Sepsis Fact Sheet, “Every year, severe sepsis strikes about 750,000 Americans. It’s been estimated that between 28 and 50 percent of these people die - far more than the number of U.S. deaths from prostate cancer, breast cancer and AIDS combined.”
- Approximately 45% of the cases of septicemia are due to Gram-positive bacteria, 45% are a result of Gram-negative bacteria, and 10% are due to fungi (mainly the yeast Candida).
Questions
Study the material in this section and then write out the answers to these questions. Do not just click on the answers and write them out. This will not test your understanding of this tutorial.
- _____ Defense regulatory chemicals that promote an inflammatory response by enabling white blood cells to leave the blood vessels and enter the surrounding tissue, by chemotactically attracting these white blood cells to the infection site, and by triggering neutrophils to release killing agents for extracellular killing. (ans)
_____ A decreased volume of circulating blood. (ans)
_____ Reduced delivery of nutrients and oxygen via the blood. This can lead to ischemia, a restriction in blood supply that results in damage or dysfunction of tissue. (ans)
_____ Respiratory failure from acute inflammation in the lungs, injury to capillaries in the alveoli of the lungs, and pulmonary edema. (ans)
_____ The formation of clots within the blood vessels throughout the body. (ans)
- inflammation
- septicemia
- chemokines
- cytokines
- DIC
- ARDS
- septic shock
- hypovolemia
- hypotension
- hypoperfusion
- Define hypotension and describe the biological mechanism behind 3 factors that contribute to hypotension. (ans)
- Define hypovolemia and describe the biological mechanism behind 3 factors that contribute to hypovolemia. (ans)
- Define hypoperfusion and describe the biological mechanism behind 3 factors that contribute to hypoperfusion. (ans)
- Describe the biological mechanism behind ARDS and how ARDS contributes to hypoperfusion. (ans)
- Define pyroptosis and state its role in inducing inflammation. (ans)
- Multiple Choice (ans)


