15.1.2.1: Staphylococcus aureus
- Page ID
- 43266

Organism
- Staphylococcus aureus is a Gram-positive coccus which forms grape-like clusters (staphylococcus)
- Catalase-positive facultative anaerobe
- Can ferment the carbohydrate mannitol
- Halotolerant (can live in up to 20% NaCl)
Habitat
- Part of the normal human flora
- Found in the nose (anterior nares) and to a lesser extent the skin
- Can survive on surfaces and in contaminated food
Source
- Infection can be endogenous (from your own flora) or exogenous (from the flora of others)
- A very common cause of nosocomial infection
- Can cause infection in a variety of body sites depending on route of entry
Epidemiology
- Occurs sporadically although occasional outbreaks are associated with specific sites, such as a gym
- Primary pathogen
- As mentioned above, one of the most common causes of nosocomial infection
Clinical Disease
- Staph. aureus can cause a wide array of infection and disease depending on the site of infection and the strain involved
- Superficial
- Carbuncles and furuncles (a.k.a. boils)
- Stye (or sty; infection of eyelid)
- Impetigo (skin infection)
- Localized
-
Mastitis (breast infection)
-
Urinary tract infection
-
- Systemic and most severe
-
Pneumonia (approximately 50% mortality rate)
-
Septicemia (mortality rate 10 – 30%)
-
Meningitis (approximately 50% mortality rate)
-
Osteomyelitis (bone infection) (relatively low, but can lead to septicemia)
-
Endocarditis (heart infection) (20 – 30%)
-
- Toxigenic
- Superficial
- Toxic shock syndrome
- Caused by toxic shock syndrome toxin (TSST) which is absorbed through an infected wound or vaginal wall
- Gene for TSST is carried on lysogenic phage
- Symptoms: fever, vomiting, red rash, extremely low blood pressure, sloughing of skin
- Has historically been associated with tampon use, but can occur in anyone infected with a Staph. aureus strain carrying the TSST gene
- Approximately 5% fatal
- Staphylococcal scalded skin syndrome (SSSS)
- Caused by exfoliative toxin which attacks zona granulosa of the epidermis
- Toxin is produced by Staph. aureus in localized, superficial infection and spreads throughout body
- Begins with blistering (often around mouth) and develops to sloughing of skin in patches in all areas of the body
- Most common in children, particularly neonates and infants
- Mortality in children ~5% with treatment, but more than 50% in adults
- Source: Clin Microbiol Rev. 1999 Apr; 12(2): 224–242. (images)
- Food poisoning
- Intoxication, not infection
- Some strains can produce an enterotoxin. If those strains are introduced into food and allowed to grow, the enterotoxin is released into the food. This usually happens when food is allowed to sit at room temperature (or warmer, but not hot) for several hours.
- When someone ingests the toxin-containing food, they develop the typical symptoms of food poisoning usually within 4 hours. Symptoms only last about 24 hours.
- Infections with non-antibiotic resistant strains are relatively easy to cure with antibiotics such as cephalosporins, other beta-lactams such as nafcillin or oxacillin, vancomycin, daptomycin, telavancin, or linezolid.
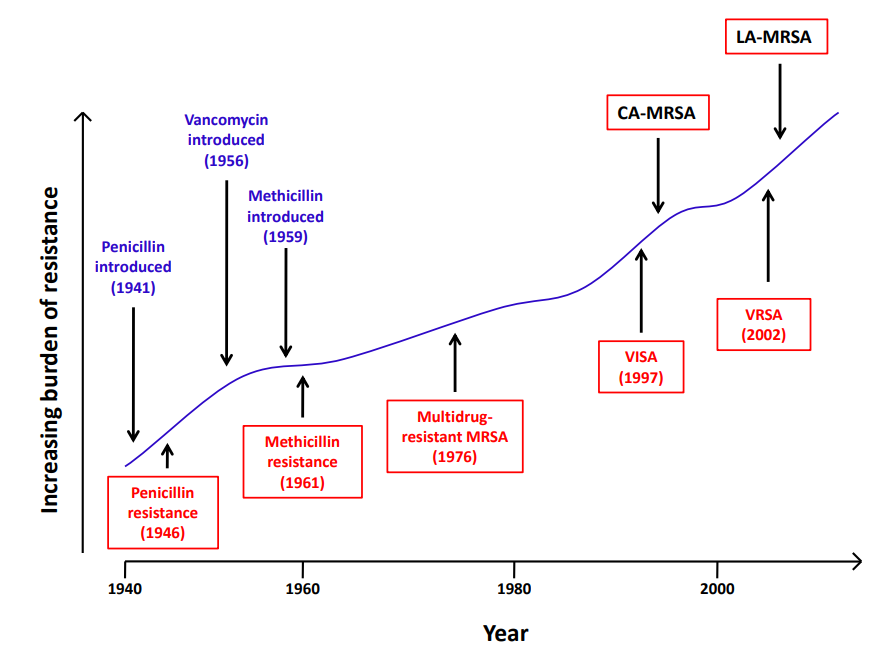
- Antibiotic resistance is a huge problem with Staph. aureus, most commonly methicillin-resistant Staph. aureus (MRSA). In addition to being resistant to methicillin, MRSA also has resistance to many other commonly used antibiotics, making MRSA infections difficult to treat. The antibiotic vancomycin is usually used to treat MRSA. Unfortunately, Staph. aureus has recently evolved resistance to vancomycin as well (VRSA) and these strains are becoming increasingly prevalent, especially in health care settings. (Figure \(\PageIndex{2}\))
- The increase of antibiotic-resistant Staph. aureus and its presence in the flora of much of the population makes it even more imperative that health care workers take precautions when caring for patients such as hand washing, wearing gloves, proper antisepsis and cleansing of patient wounds, and good aseptic technique when inserting in-dwelling devices. Proper education of patients for the prudent use of antibiotics is also critical.
Primary Virulence Factors
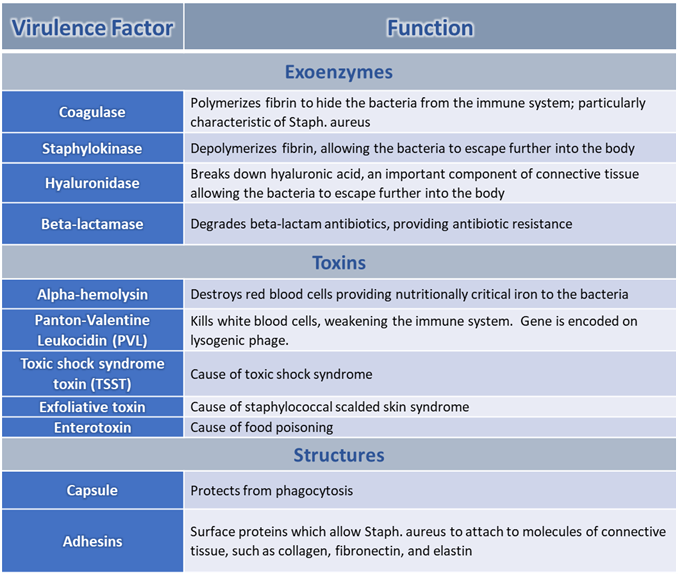
- Staph. aureus has a variety of virulence factors which allow it to invade the body, attach to tissues, and grow. (Figures \(\PageIndex{3}\) and \(\PageIndex{4}\))
- Some virulence factors, such as TSST, exfoliative toxin, and enterotoxin, are only produced by some strains
- The genes for strain-specific virulence factors are often carried on lysogenic phages or plasmids
Figure \(\PageIndex{3}\): Staphylococcus aureus cell structure and pathogenic factors. Staphylococcus aureus has a complex cell wall structure composed of a thick peptidoglycan layer and polysaccharide capsule. In addition, S. aureus possesses an elaborate arsenal of structural and secreted virulence factors involved in toxin production, adherence to and invasion of host tissue, and immune evasion. (2016;Eric F. Kong,Jennifer K. Johnson, and Mary Ann Jabra-Rizk; doi: 10.1371/journal.ppat.1005837
Additional Information: http://textbookofbacteriology.net/staph.html

