6.6: Disorders of the Muscular System
- Last updated
- Save as PDF
- Page ID
- 30655
Pain in the Neck
Spending hours each day looking down at hand-held devices is a pain in the neck — literally. The weight of the head bending forward can put a lot of strain on neck muscles, and muscle injuries can be excruciating. Neck pain is one of the most common complaints that bring people to the doctor’s office. In any given year, about one in five adults will suffer from neck pain. That’s a lot of pain in the neck! Not all of them are due to muscular disorders, but many of them are. Muscular disorders, in turn, generally fall into two general categories: musculoskeletal disorders and neuromuscular disorders.

Musculoskeletal Disorders
Musculoskeletal disorders are injuries in muscles or associated tissues (such as tendons) because of biomechanical stresses. They may be caused by sudden exertion, over-exertion, repetitive motions, or long periods of maintaining awkward positions. Musculoskeletal disorders often work- or sports-related, and generally, just one or a few muscles are affected. They can often be treated successfully, and full recovery can be very likely. The disorders include muscle strains, tendonitis, and carpal tunnel syndrome.
Muscle Strain
A muscle strain is an injury in which muscle fibers tear as a result of overstretching. A muscle strain is also commonly called a pulled muscle or torn muscle. (Strains are often confused with sprains, which are similar injuries to ligaments.) Depending on the degree of injury to muscle fibers, a muscle strain can range from mildly to extremely painful. Besides pain, typical symptoms include stiffness and bruising in the area of the strained muscle. Figure \(\PageIndex{2}\) shows a large bruise caused by a hamstring muscle strain. Hamstring strains are prevalent in track and field athletes. In sprinters, for example, about one-third of injuries are hamstring injuries. Having a previous hamstring injury puts an athlete at increased risk of having another one.

Proper first aid for a muscle strain includes five steps, which are represented by the acronym PRICE. The PRICE steps should be followed for several days after the injury. The five steps are:
- Protection: Apply soft padding to the strained muscle to minimize impact with objects that might cause further damage.
- Rest: Rest the muscle to accelerate healing and reduce the potential for re-injury.
- Ice: Apply ice for 20 minutes at a time every two hours to reduce swelling and pain.
- Compression: Apply a stretchy bandage to the strained muscle to reduce swelling.
- Elevation: Keep the strained muscle elevated to reduce the chance of blood pooling in the muscle.
Non-steroidal anti-inflammatory drugs (NSAIDs, such as ibuprofen) can help reduce inflammation and relieve pain. However, because such drugs interfere with blood clotting, they should be taken only after bleeding in the muscle has stopped — not immediately after the injury occurs. For severe muscle strains, professional medical care may be needed.
Tendinitis
Tendinitis is inflammation of a tendon that occurs when it is over-extended or worked too hard without rest. Tendons that are commonly affected include those in the ankle, knee, shoulder, and elbow. The affected tendon depends on the type of use that causes inflammation. Rock climbers tend to develop tendinitis in their fingers, while basketball players are more likely to develop tendonitis in the knees, to name a few examples.
Symptoms of tendinitis may include aching, sharp pain, a burning sensation, or joint stiffness. In some cases, swelling occurs around the inflamed tendon, and the area feels hot and looks red. Treatment includes the PRICE guidelines listed above and the use of NSAIDs to reduce inflammation and pain further. Although symptoms should show improvement within a few days of treatment, full recovery may take several months. A gradual return to exercise or other use of the affected tendon is recommended. Physical or occupational therapy may speed the return to normal activity levels.
Carpal Tunnel Syndrome
Carpal tunnel syndrome is a common biomechanical problem in the wrist when the median nerve becomes compressed between carpal bones (Figure \(\PageIndex{3}\)). This may occur due to repetitive use of the wrist, a tumor, or trauma to the wrist. Two-thirds of the cases are work-related. Computer work, work with vibrating tools and work requiring a strong grip all increase one's risk of developing this problem. Carpal tunnel syndrome occurs more often in women than in men. Other risk factors include obesity, pregnancy, and arthritis. Genetics may also play a role.
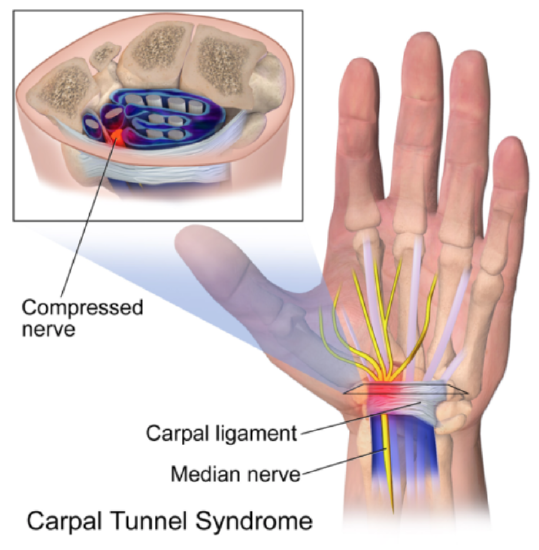
Compression of the median nerve results in the muscles' inadequate nervous stimulation in the thumb and first two fingers of the hand. The main symptoms are pain, numbness, and tingling in these digits. Sometimes, symptoms can be improved by wearing a wrist splint or receiving corticosteroid injections. Surgery to cut the carpal ligament reduces pressure on the median nerve and is generally more effective than nonsurgical treatment. Recurrence of carpal tunnel syndrome after surgery is rare. On the other hand, without treatment, the lack of nervous stimulation by the median nerve may eventually cause the affected muscles of the hand to weaken and waste away.
Neuromuscular Disorders
Neuromuscular disorders are systemic disorders that occur because of problems with the nervous control of muscle contractions or muscle cells themselves. These disorders are often due to faulty genes and not due to biomechanical stresses. Other system-wide problems, such as abnormal immune system responses, may also be involved in neuromuscular disorders.
Unlike musculoskeletal disorders, neuromuscular disorders generally affect most or all of the muscles in the body. The disorders also tend to be progressive and incurable. However, in most cases, treatment is available to slow the disease progression or lessen symptoms. Examples of neuromuscular disorders include muscular dystrophy, myasthenia gravis, and Parkinson’s disease.
Muscular Dystrophy
Muscular dystrophy is a genetic disorder caused by defective proteins in muscle cells. It is characterized by progressive skeletal muscle weakness and death of muscle cells and tissues. Muscles become increasingly unable to contract in response to nervous stimulation.
There are at least nine major types of muscular dystrophy caused by different gene mutations. Some of the mutations cause autosomal recessive or autosomal dominant disorders, and some cause X-linked disorders. The most common type of childhood muscular dystrophy is Duchenne muscular dystrophy (DMD) due to a mutation in a recessive gene on the X chromosome. As an X-linked recessive disorder, Duchenne muscular dystrophy occurs almost exclusively in males.
Different types of muscular dystrophy affect different major muscle groups. In Duchenne muscular dystrophy, the lower limbs are affected. Signs of the disorder usually first become apparent when a child starts walking. Difficulty walking becomes progressively worse through childhood. By the time a child is ten, braces may be needed for walking — and walking may no longer even be possible by age 12. The lifespan of someone with muscular dystrophy is likely to be shorter than normal because of the disease, ranging from 15 to 45 years.
Duchenne muscular dystrophy (DMD) is a progressive weakening of the skeletal muscles. It is one of several diseases collectively referred to as “muscular dystrophy.” DMD is caused by a lack of the protein dystrophin, which helps the thin filaments of myofibrils bind to the sarcolemma. Without sufficient dystrophin, muscle contractions cause the sarcolemma to tear, causing an influx of Ca++, leading to cellular damage and muscle fiber degradation. Over time, as muscle damage accumulates, muscle mass is lost, and greater functional impairments develop.
In some cases, physical therapy, drug therapy, or orthopedic surgery may improve muscular dystrophy signs and symptoms. However, at present, there is no known cure for the disorder. Research is ongoing to find a cure, with financial support from such sources as the Muscular Dystrophy Association (MDA) (see photo below). MDA is a non-profit organization dedicated to curing muscular dystrophy by funding worldwide research.

Myasthenia Gravis
Myasthenia gravis is an autoimmune disorder in which circulating antibodies block the nicotinic acetylcholine receptors on the neuromuscular junction's motor endplate. This blockage of acetylcholine receptors causes muscle weakness, often first exhibiting drooping eyelids and expanding to include overall muscle weakness and fatigue. It occurs more commonly in women and generally begins between the ages of 20 and 40. The initial symptom of myasthenia gravis is painless muscle weakness, generally in muscles around the eye (Figure \(\PageIndex{5}\)). The disease then progresses to muscles elsewhere in the body, eventually involving most of the muscles. Swallowing and chewing may become difficult as the disease progresses, and speech may become slow and slur. In more advanced cases, myasthenia crises may occur, during which the muscles that control breathing may be affected. Emergency medical care to provide assisted ventilation is required to sustain life. A myasthenia gravis crisis may be triggered by various stressors, such as infection, fever, or stress. Treatment of myasthenia gravis may include medications to counter the mutant gene's effects or suppress the immune system.

Parkinson’s Disease
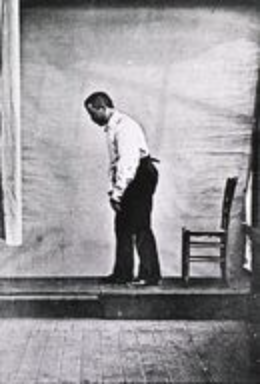
Parkinson’s disease is a degenerative disorder of the central nervous system that mainly affects the muscular system and movement. Four motor signs and symptoms are considered defining Parkinson’s disease: muscle tremor (shaking), muscle rigidity, slowness of movement, and postural instability. Tremor is the most common and obvious symptom, and it most often occurs in a limb at rest, so it disappears during sleep or when the patient moves the limb voluntarily. Difficulty walking eventually develops, and dementia is common in the advanced stages of the disease. Depression is common, as well.
Parkinson’s disease is more common in older people, with most cases being diagnosed after 50. Often, the disease occurs for no known reason. Cases like this are called primary Parkinson’s disease. Sometimes, the disease has a known or suspected cause, such as exposure to toxins in pesticides or repeated head trauma. In this case, it is called secondary Parkinson’s disease. Regardless of the cause, the disease's motor symptoms result from the death of neurons in the midbrain. The cause of cell death is not fully understood, but it appears to involve the buildup in the brain of protein structures called Lewy bodies. Early in the course of the illness, medications can be prescribed to help reduce the motor disturbances. As the disease progresses, however, the medications become ineffective. They also cause a negative side effect of involuntary writhing movements.
Feature: Human Biology in the News
On June 3, 2016, media worldwide exploded with news of the death of Muhammad Ali at the age of 74. The world champion boxer and Olympic gold medalist died that day of a respiratory infection complication, but the underlying cause was Parkinson’s disease. Ali was diagnosed with Parkinson’s in 1984 when he was only 42 years old. Doctors attributed his disease to repeated head trauma from boxing.
In the days following Ali’s death, the news was full of stories and images from milestones in the athlete’s life, both before and after his diagnosis with Parkinson’s disease. Sadly, the news coverage also provided an overview of his gradual decline as the disease progressed. Ali was pictured in 1996, lighting the flame at the Summer Olympics in Atlanta. In 2012, Ali had to be helped to his feet by his wife to stand before the flag he was supposed to carry into the stadium. He was unable to carry it because of the ravages of Parkinson’s disease.
Muhammad Ali retired from boxing in 1981 at 39, but he didn’t retire from fighting. Until the final year of his life, Ali was a passionate activist for peace and justice and against war and racism. In 1998, he joined Michael J. Fox, who also has Parkinson’s disease, to raise awareness and fund research on Parkinson’s disease. In 2002, Fox and Ali made a joint appearance before Congress to present their case. In 2005, Ali received the Presidential Medal of Freedom from George W. Bush (Figure \(\PageIndex{7}\)) for the many achievements and contributions he made throughout his amazing life, despite Parkinson’s disease.

Review
- What are musculoskeletal disorders? What causes them?
- How does a muscle strain occur?
- Define tendinitis. Why does it occur?
- Identify first-aid steps for treating musculoskeletal disorders such as muscle strains and tendinitis.
- Describe carpal tunnel syndrome and how it may be treated.
- Define neuromuscular disorders.
- Identify the cause and symptoms of muscular dystrophy.
- Outline the cause and progression of myasthenia gravis.
- What is Parkinson’s disease? List four characteristic signs of the disorder.
- What are the main differences between musculoskeletal disorders and neuromuscular disorders?
- Why is the padding of a strained muscle part of the typical treatment?
- Which disorder would be the most likely to be caused by repeated use of a jackhammer?
A. Parkinson’s disease
B. Muscular dystrophy
C. Carpal tunnel syndrome
D. A neuromuscular disorder
- True or False. Participation in some sports may cause Parkinson’s disease.
- True or False. Myasthenia gravis occurs because the body stops making acetylcholine.
- What are two tissues, other than muscle tissue, that can experience problems that result in muscular system disorders?
Explore More
Attributions
- Meet and Tweet by Alliance Internationale, CC BY 2.0 via Wikimedia Commons
- Pulled Hamstring by Daniel.Cardenas, CC BY 3.0 via Wikimedia Commons
- Carpal Tunnel Syndrome by Blausen.com staff (2014). "Medical gallery of Blausen Medical 2014". WikiJournal of Medicine 1 (2). DOI:10.15347/wjm/2014.010. ISSN 2002-4436. licensed CC BY 3.0 via Wikimedia Commons
- Fill the boot by USMC, public domain via Wikimedia Commons
- Myasthenia gravis by Mohankumar Kurukumbi, Roger L Weir, Janaki Kalyanam, Mansoor Nasim, Annapurni Jayam-Trouth. CC BY 2.0 via Wikimedia Commons
- Paralysis agitans by Albert Londe, public domain via Wikimedia Commons
- Muhammad Ali and President Bush, White House photo by Paul Morse, public domain via Wikimedia Commons
- Text adapted from Human Biology by CK-12 licensed CC BY-NC 3.0


