15.3: Infectious Diseases
- Page ID
- 31633
Worldwide, infectious diseases (biological hazards) accounted for three of the 10 leading causes of death in 2020. In children under five leading causes of death include acute respiratory infections (from indoor air pollution); diarrheal diseases (mostly from poor water, sanitation, and hygiene); and other infectious diseases such as malaria. Children are especially susceptible to environmental factors that put them at risk of developing illness early in life. Malnutrition (the condition that occurs when body does not get enough nutrients) is an important contributor to child mortality—malnutrition and environmental infections are inextricably linked.
The World Health Organization (WHO) recently concluded that about 50% of the consequences of malnutrition are in fact caused by inadequate water and sanitation provision and poor hygienic practices. For example, intestinal worms, which thrive in poor sanitary conditions, infect close to 90 percent of children in the developing world and, depending on the severity of the infection may lead to malnutrition, anemia, or stunted growth. About 6 million people are blind from trachoma, a disease caused by the lack of clean water combined with poor hygiene practices.
An emerging infectious disease is either new to the human population or has shown an increase in prevalence in the previous twenty years. Examples include coronavirus disease 19 (COVID-19), Ebola virus disease, West Nile virus, Zika virus, sudden acute respiratory syndrome (SARS), H1N1 influenza; swine and avian influenza (swine, bird flu), human immunodeficiency virus (HIV)/acquired immunodeficiency disorder (AID, and a variety of other viral, bacterial, and protozoal diseases (table \(\PageIndex{a}\)). Whether the disease is new or conditions have changed to cause an increase in frequency, its status as emerging implies the need to apply resources to understand and control its growing impact. Emerging diseases may change their frequency gradually over time, or they may experience sudden widespread growth.
| Disease | Pathogen | Year Discovered | Affected Regions | Transmission |
|---|---|---|---|---|
| AIDS | HIV | 1981 | Worldwide | Contact with infected body fluids |
| Chikungunya fever | Chikungunya virus | 1952 | Africa, Asia, India; spreading to Europe and the Americas | Mosquito-borne |
| Ebola virus disease | Ebola virus | 1976 | Central and Western Africa | Contact with infected body fluids |
| H1N1 Influenza (swine flu) | H1N1 virus | 2009 | Worldwide | Droplet transmission |
| Lyme disease | Borrelia burgdorferi bacterium | 1981 | Northern hemisphere | From mammal reservoirs to humans by tick vectors |
| West Nile virus disease | West Nile virus | 1937 | Africa, Australia, Canada to Venezuela, Europe, Middle East, Western Asia | Mosquito-borne |
Emerging diseases are found in all countries, both developed and developing. Some nations are better equipped to deal with them. National and international public health agencies watch for epidemics in developing countries because those countries rarely have the health-care infrastructure and expertise to deal with large outbreaks effectively. In addition to the altruistic goal of saving lives and assisting nations lacking in resources, the global nature of transportation means that an outbreak anywhere can spread quickly to every corner of the planet. Managing an epidemic in one location—its source—is far easier than fighting it on many fronts.
In 2015, the WHO set priorities on several emerging diseases that had a high probability of causing epidemics and that were poorly understood (and thus urgently required research and development efforts).
A reemerging infectious disease is a disease that is increasing in frequency after a previous period of decline. Its reemergence may be a result of changing conditions or old prevention regimes that are no longer working. Examples of such diseases are drug-resistant forms of tuberculosis, bacterial pneumonia, and malaria. Drug-resistant strains of the bacteria causing gonorrhea and syphilis are also becoming more widespread, raising concerns of untreatable infections.
A variety of environmental factors may contribute to re-emergence of a particular disease, including temperature, moisture, human food or animal feed sources, etc. Disease re-emergence may be caused by the coincidence of several of these environmental and/or social factors to allow optimal conditions for transmission of the disease.
It seems likely that a wide variety of infectious diseases have affected human populations for thousands of years emerging when the environmental, host, and agent conditions were favorable. Expanding human populations have increased the potential for transmission of infectious disease as a result of close human proximity and increased likelihood for humans to be in “the wrong place at the right time” for disease to occur (eg, natural disasters or political conflicts). Global travel increases the potential for a carrier of disease to transmit infection thousands of miles away in just a few hours, as evidenced by WHO precautions concerning international travel and health.
Selected Infectious Diseases
COVID-19
Coronavirus disease 19 (COVID-19) is a respiratory illness caused by a virus called novel species of coronavirus (SARS-CoV-2). Symptoms include fever or chills, cough, shortness or breath or difficulty breathing, fatigue, headache, and sore throat. The WHO declared coronavirus disease 19 (COVID-19) a public health emergency of international concern on January 30 and a pandemic on March 11, 2020. A seemingly limited cluster of cases of pneumonia linked to a sea food market in Wuhan, China has become one of the worst pandemics in human history with a staggering number of more than 90.2 million infections in 177 countries and 1.9 million deaths globally as of January 10, 2021 (figure \(\PageIndex{a}\)). This illustrates how locally emerging pathogens have the capacity to spread rapidly and cross borders and become an imminent public health threat to the entire world. You can view the the latest COVID-19 data here.
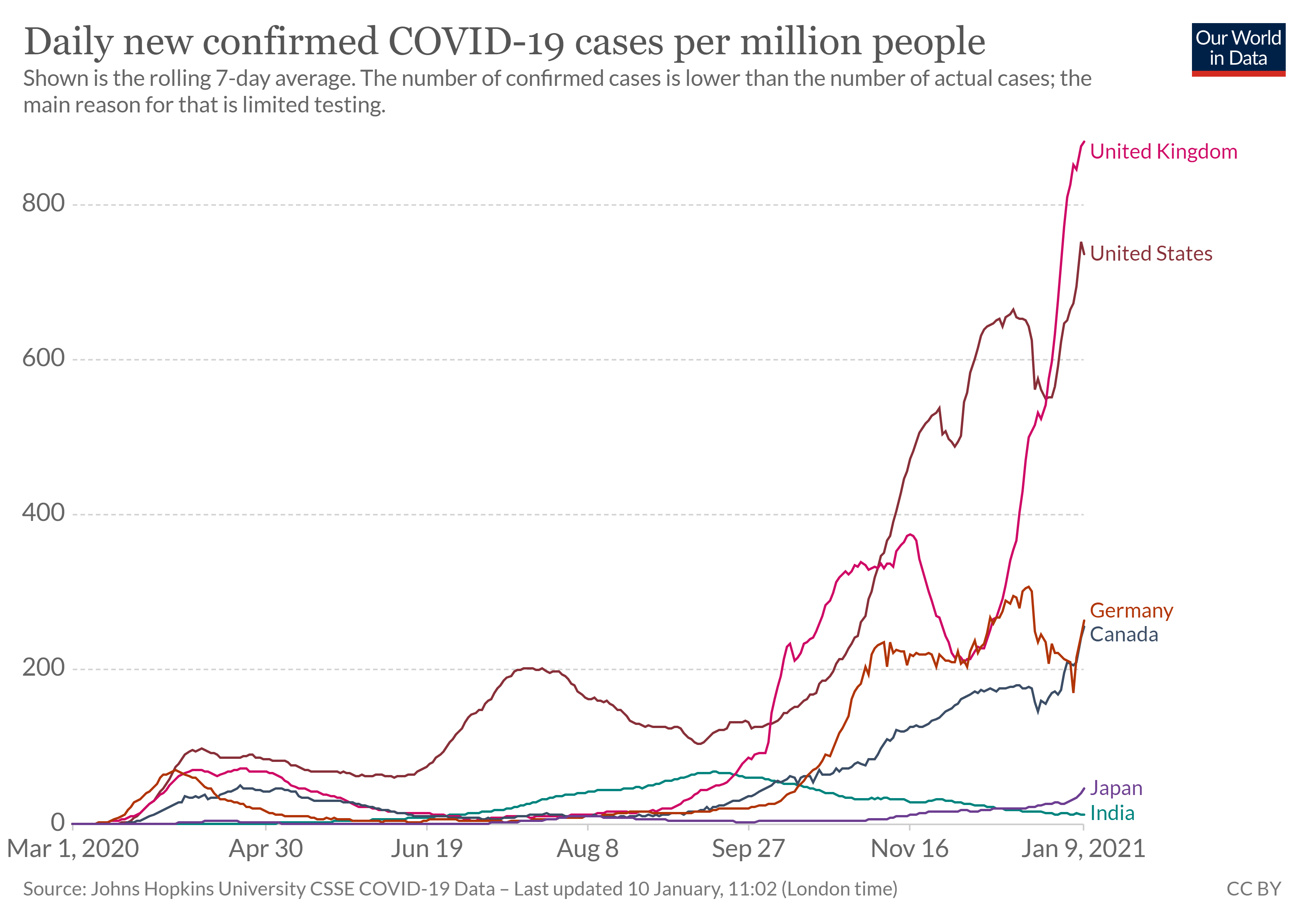
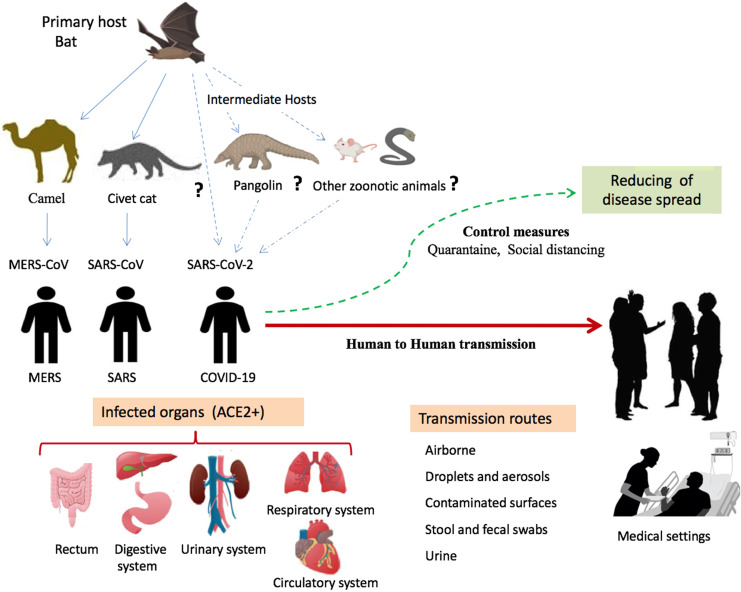
Studies indicate that SARS-CoV-2 might originate from bat coronaviruses and infects humans directly or through other animals as intermediaries. It primarily spreads between humans through the respiratory tract by involving droplets, aerosols, respiratory secretions, or saliva. It is most often spread by direct contact transmission, but it airborne transmission has been documented in certain situations, such as in an enclosed space (figure \(\PageIndex{b}\)). Researchers continue to investigate airborne transmission of the virus. This coronavirus is infectious during its incubation period, which is reported to be 3-7 days, at most 14 days, when no symptoms are shown in patients. Those infected may experience mild to moderate disease (80%), severe disease (15%), and critical illness (5%) with an overall case fatality rate of 0.5–2.8% with much higher rates (3.7–14.8%) in octogenarians. The severe and critical illness categories (about 20% of all infections) have overwhelmed health systems worldwide (figure \(\PageIndex{c}\)). The Centers for Disease Control and Prevention's COVID-19 page has the latest information about preventing transmission, vaccines, symptoms, and testing.

Ebola Virus Disease
Ebola virus disease, previously known as Ebola hemorrhagic fever, is a rare and deadly disease caused by infection with one of the Ebola virus strains (figure \(\PageIndex{d}\)). Ebola can cause disease in humans and nonhuman primates. Health experts had been aware of the Ebola virus since the 1970s, but outbreak at scale that had not yet been seen occurred in western Africa through 2014–2016. Previous human epidemics had been small, isolated, and contained. Indeed, the gorilla and chimpanzee populations of western Africa had suffered far worse from Ebola than the human population. The pattern of small isolated human epidemics changed in 2014. Its high transmission rate, coupled with cultural practices for treatment of the dead and perhaps its emergence in an urban setting, caused the disease to spread rapidly, and thousands of people died. The international public health community responded with a large emergency effort to treat patients and contain the epidemic.
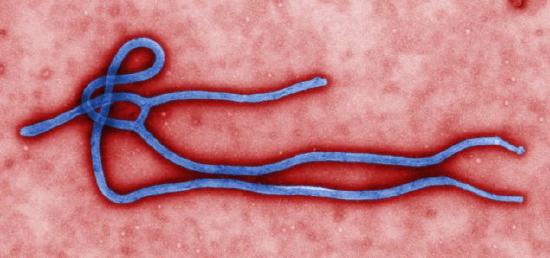
The 2014-2016 Ebola epidemic was the largest in history (with 28,616 cases and 11,310 deaths), affecting multiple countries in West Africa. There were a small number of cases reported in Nigeria and Mali and a single case reported in Senegal; however, these cases were contained, with no further spread in these countries. Even with the support of international agencies, the systems in western Africa struggled to identify and care for the sick and control spread. Engaging local leaders in prevention programs and messaging, along with careful policy implementation at the national and global level, helped to eventually contain the spread of the virus and put an end to this outbreak. The U.S. Food and Drug Administration approved a vaccine for Ebola late in 2019.
HIV/AIDS
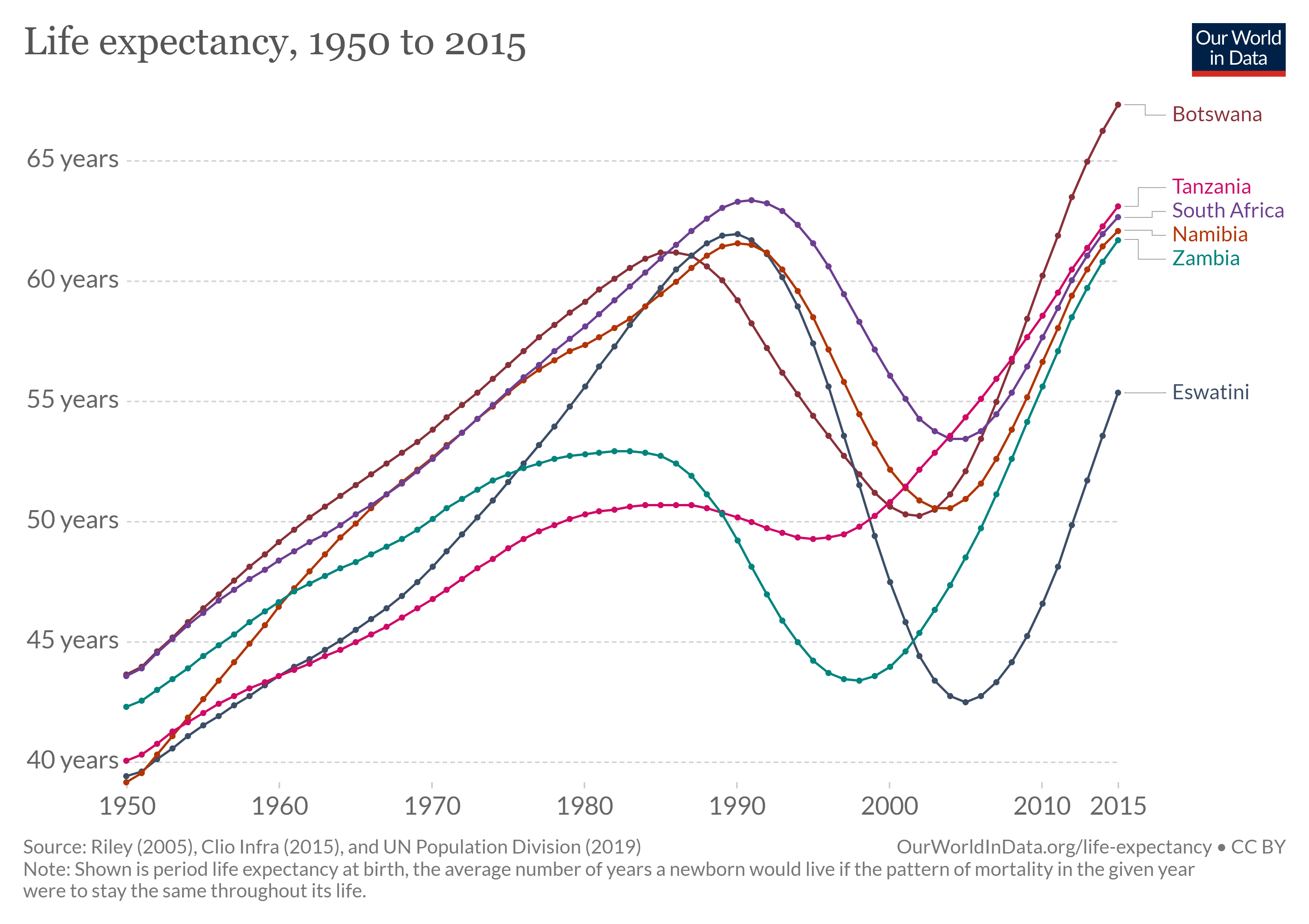
Human immunodeficiency virus (HIV) is a virus that attacks the body’s immune system. If HIV is not treated, it can lead to acquired immunodeficiency syndrome (AIDS). Those with AIDS have weakened immune systems and are thus more susceptible to cancers and other infections. First identified in 1981, the HIV/AIDS epidemic has spread with ferocious speed. In 2019, 38 million people were living HIV globally. Over 95 percent of people living with HIV are in low- and middle- income countries. There were 1.7 million new infections in 2019, and more than half of new infections are among young people below age 25. In 2019 alone, 690,000 million people died from AIDS and related illnesses. In 2016, HIV/AIDS is was the second leading cause of death in Africa. At its peak, the epidemic cut life expectancy by more than 10 years in several nations (figure \(\PageIndex{e}\)).
Malaria
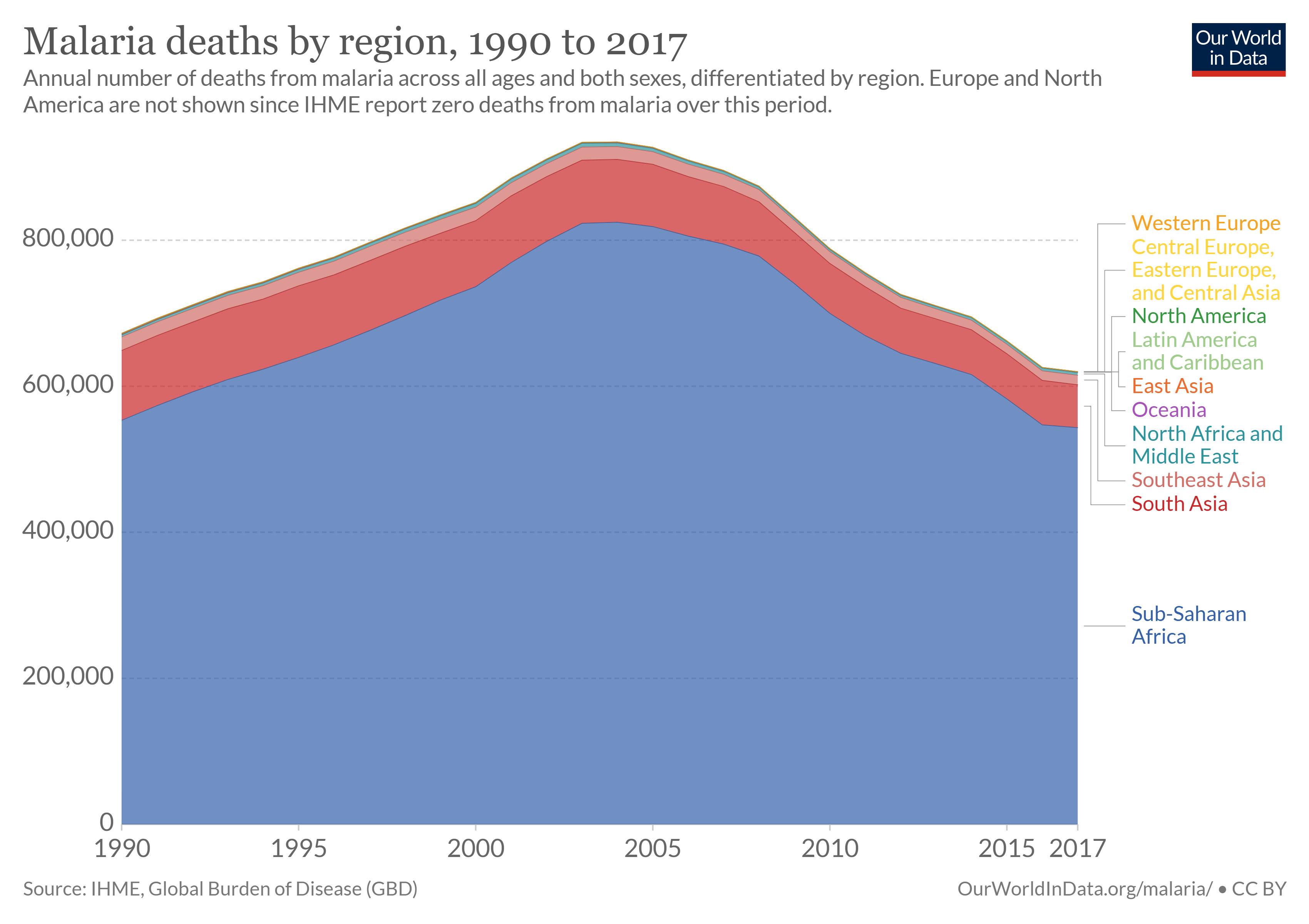
Approximately 40% of the world’s people—mostly those living in the world’s poorest countries—are at risk from malaria. Malaria is an infectious disease spread by mosquitoes but caused by a single-celled protozoan parasite called Plasmodium. There were 229 million cases of malaria and 409,000 deaths in 2019 with most cases and deaths found in Sub-Saharan Africa (figure \(\PageIndex{f}\)). However, Asia, Latin America, the Middle East, and parts of Europe are also affected. Pregnant women are especially at high risk of malaria. Non-immune pregnant women risk both acute and severe clinical disease, resulting in fetal loss in up to 60% of such women and maternal deaths in more than 10%, including a 50% mortality rate for those with severe disease. Semi-immune pregnant women with malaria infection risk severe anemia (lack of sufficient red blood cells to deliver oxygen) and impaired fetal growth, even if they show no signs of acute clinical disease. An estimated 10,000 women and 200,000 infants die annually as a result of malaria infection during pregnancy.
Tuberculosis
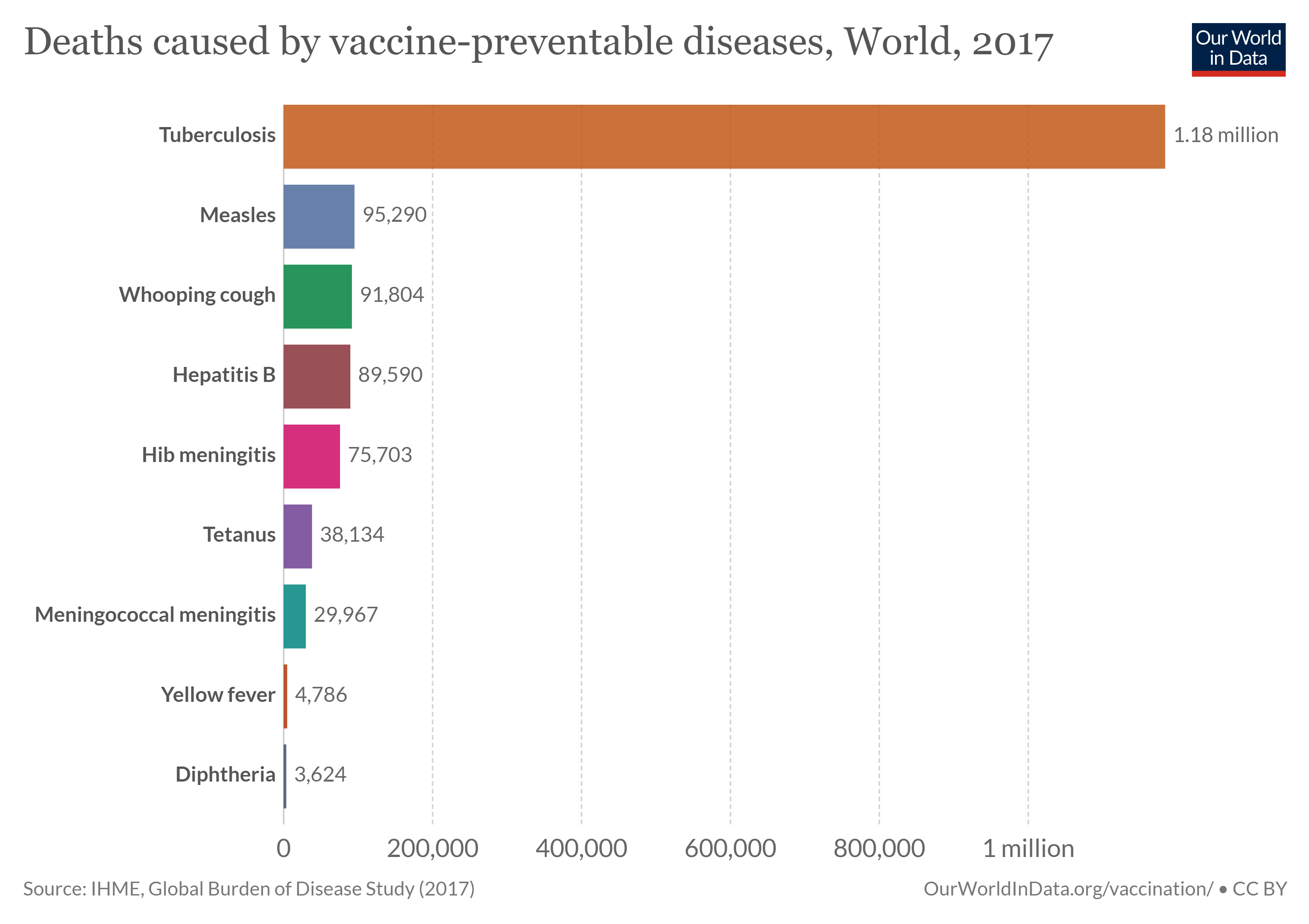
The WHO estimates that 10.4 million new cases and 1.5 million deaths occur from tuberculosis (TB) each year. One-third of TB cases remain unknown to the health care system. For those accessing treatment, however, prevalence and mortality have declined significantly, and millions of lives have been saved.
Tuberculosis is caused by the bacterium Mycobacterium tuberculosis, which is transmitted between humans through the respiratory route and most commonly affects the lungs but can damage any tissue. When an infected individual coughs, exhales, speaks, etc., the bacterium is released in droplets that can remain suspended in the air for several hours. Only a minority (approximately 10 percent) of individuals infected with M. tuberculosis progress to active TB disease, while the remainder may maintain a latent infection that serves as a reservoir. TB has special challenges, including (a) a substantial number of patients with active disease are asymptomatic, capable of transmitting infection without knowing it; (b) patients must maintain compliance with treatment for six to nine months; and (c) the pathogen persists in many infected individuals in a latent state for many years but can be reactivated over a lifetime to cause disease and become transmissible.
This video by the CDC explains the basics of TB.
Disease Eradication
Many diseases have been eradicated or are nearly eradicated worldwide (Table \(\PageIndex{b}\)). Strategies to eradicate disease infectious diseases include vaccination, improved hygiene and sanitation, preventative medication, and public health education. Some of these strategies are discussed in Environmental Health Reduction, and vaccination is discussed below.
| Disease | Burden of disease | Cause | Ways to eradicate | Fatality |
|---|---|---|---|---|
| Smallpox | Declared eradicated in 1980 | Variola virus | Eradicated using vaccination | 30% |
| Rinderpest | Declared eradicated in 2011 | Rinderpest virus | Sanitary measures and vaccination | 100% |
| Poliomielitis | 116 cases in 2017 | Poliovirus | Vaccination | For paralytic polio 2-5% in children and increases to 15-30% in adults |
| Guinea worm disease | 30 cases in 2017 | Parasitic worm Dracunculus medinensis | Hygiene, water decontamination and health education | Not fatal but debilitating |
| Measles | 173,457 reported cases to WHO in 2017 | Measles morbillivirus | Vaccination | 15% |
| Mumps | 560,622 reported cases to WHO in 2017 | Mumps orthorubulavirus | Vaccination | 0.01% for mumps-caused encephalitis |
| Rubella | 6,789 reported cases to WHO in 2017 | Rubella virus | Vaccination | Not reported |
| Lymphatic filariasis | No estimate available. In 2014, 68 million people were infected and 790 million people where at risk of infection | Roundworms: W. bancrofti, B. malayi, B. timori |
Preventive chemotherapy | Not fatal but highly debilitating |
| Cysticercosis | 2.56–8.30 million cases estimated by the WHO | Tapeworms: T. solium, T. saginata, T. asiatica |
Sanitation and health education. Vaccination of pigs | Varies between countries <1-30% |
Table modified from Max Roser, Sophie Ochmann, Hannah Behrens, Hannah Ritchie and Bernadeta Dadonaite (2014) - "Eradication of Diseases". Published online at OurWorldInData.org. (CC-BY).
Vaccination
Vaccines function in inducing a specific immune response that can immediately counter a pathogen if exposed. Vaccines lead to the production of specialized cells and antibodies, which can efficiently and effectively target pathogens. There are several types of vaccines. Some consists of dead or inactivated pathogens or parts of them. The Pfizer-BioNTech and Moderna COVID-19 vaccines, approved by the FDA in December of 2020 consist of a piece of the the virus's genetic material (called mRNA). When injected, the body uses this genetic information to synthesize the spike protein of the virus, which stimulates an immune responses without causing infection.
Development and approval of a vaccine does not automatically eradicate a disease (figure \(\PageIndex{g}\)), for the vaccine must be distributed to those who need it. Access is particularly challenging in developing countries, especially for low-income individuals there. In the case of tuberculosis, which remains widespread, a vaccine has been available for 100 years, but it is more effective in protecting severe forms of the disease in children than lung infections in adults. A new, more effective vaccine is likely needed to eradicate tuberculosis.
New vaccines must be rigorously tested before they are approved. Not only are vaccines safe, but we would face spikes in deadly infectious diseases without them. The antivax movement has unfortunately spread false information questioning the safety of vaccines, but you can educate yourself with reliable information about the development, testing, and safety of vaccines here.
Antibiotic Resistance
Antibiotics and similar drugs, together called antimicrobial agents, have been used for the last 70 years to treat patients who have infectious diseases. Technically, antibiotics are substances that are produced by certain microorganisms (such as the fungus, Penicillium, or the bacterium Streptomyces) that inhibit the growth of other microorganisms. However, any drugs used to treat bacterial infections are commonly referred to as antibiotics. Neither of these definitions includes substances used to treat viral infections, which are called antivirals. Since the 1940s, the use of antiobitics has greatly reduced illness and death from infectious diseases. However, these drugs have been used so widely and for so long that the infectious organisms the antibiotics are designed to kill have adapted to them, making the drugs less effective.
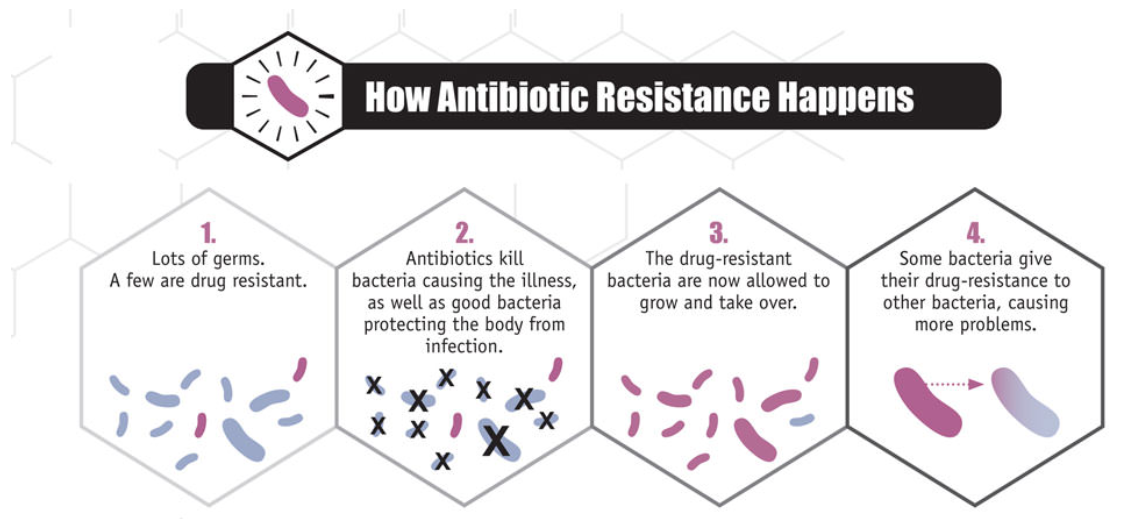
Overuse of antibiotics have allowed pathogens to evolve antibiotic resistance, which occurs when bacteria change in a way that reduces the effectiveness of drugs, chemicals, or other agents designed to cure or prevent infections (figure \(\PageIndex{h}\)). Overuse takes many forms, such as the inclusion of antibiotics in household products or prescribing antibiotics to treat infections without first determining whether the infection is bacterial or viral (in which case, the antibiotic would not be effective). Similar to the evolution of pesticide resistance, widespread use of antibiotics favors individuals that happen to have gene versions conferring antibiotic resistance. These individuals have the best chance of surviving and reproducing, so much so, that an antibiotic-resistant strain evolves. The initial antibiotic is not longer effective against this strain, and it must be treated with alternative medications. For example, tuberculosis (TB) was nearly eliminated in most parts of the world, but drug-resistant strains have now reversed that trend.
A similar example of drug resistance has evolved in Plasmodium, the protozoa that cause malaria. The insecticide dichlorodiphenyltrichloroethane (DDT) was widely used to control malaria-carrying mosquito populations in tropical regions. However, after many years the mosquitoes developed a natural resistance to DDT and again spread the disease widely. Anti-malarial medicines were also over-prescribed, which allowed Plasmodium to become drug-resistant.
New forms of antibiotic resistance can cross international boundaries and spread between continents with ease. Many forms of resistance spread with remarkable speed. Each year in the United States, at least 2 million people acquire serious infections with bacteria that are resistant to one or more of the antibiotics designed to treat those infections. At least 23,000 people die each year in the US as a direct result of these antibiotic-resistant infections. Many more die from other conditions that were complicated by an antibiotic-resistant infection. The use of antibiotics is the single most important factor leading to antibiotic resistance around the world. Antibiotics are among the most commonly prescribed drugs used in human medicine, but up to 50% of all the antibiotics prescribed for people are not needed or are not optimally effective as prescribed.
The video below shows an experiment done at Harvard Medical school, where they show bacteria adapting very quickly to apparently deadly conditions.
During recent years, there has been growing concern over methicillin-resistant Staphylococcus aureus (MRSA), a bacterium that is resistant to many antibiotics. In the community, most MRSA infections are skin infections. In medical facilities, MRSA causes life-threatening bloodstream infections, pneumonia and surgical site infections.
Attribution
Modified by Melissa Ha from the following sources:
- Environmental Health and Sustainable Agriculture from Environmental Biology by Matthew R. Fisher (licensed under CC-BY)
- Environmental Health and Child Survival: Epidemiology, Economics, Experiences. Environment and Development. 2008. World Bank. Washington, DC. CC-BY.
- Global Public Health from Microbiology by OpenStax (CC-BY). Access for free at openstax.org.
- Patel, V., D. Chisholm., T. Dua, R. Laxminarayan, and M. E. Medina-Mora, editors. 2015. Mental, Neurological, and Substance Use Disorders. Disease Control Priorities, third edition, volume 4. Washington, DC: World Bank. doi:10.1596/978-1-4648-0426-7. (CC-BY).
- Balkhair A. A. 2020. COVID-19 Pandemic: A New Chapter in the History of Infectious Diseases. Oman medical journal, 35(2), e123. https://doi.org/10.5001/omj.2020.41 (CC-BY-NC).
- Tizaoui, K., Zidi, I., Lee, K. H., Ghayda, R. A., Hong, S. H., Li, H., Smith, L., Koyanagi, A., Jacob, L., Kronbichler, A., & Shin, J. I. (2020). Update of the current knowledge on genetics, evolution, immunopathogenesis, and transmission for coronavirus disease 19 (COVID-19). International journal of biological sciences, 16(15), 2906–2923. https://doi.org/10.7150/ijbs.48812 (CC-BY).
- Ebola (Ebola Virus Disease). 2020. Centers for Disease Control and Prevention. Accessed 10 January 2021. (public domain)
- 2014-2016 Ebola Outbreak in West Africa. 2019. Centers for Disease Control and Prevention. Accessed 10 January 2021. (public domain)
- About HIV. 2020. Centers for Disease Control and Prevention. Accessed 10 January 2021. (public domain)
- HIV/AIDS at a glance. 2003. World Bank. Washington, DC. CC-BY.


